J Korean Soc Spine Surg.
2001 Dec;8(4):497-503.
Posterior Short-Segment Instrumentation of Thoracic and Lumbar Bursting Fractures: Retrospective study related with Load-Sharing classification
- Affiliations
-
- 1Department of Orthopaedic Surgery, College of Medicine, Dong-A University, Pusan, Korea. gylee@daunet.donga.ac.kr
Abstract
-
STUDY DESIGN: The authors designed the retrospective study with the Load-Sharing Classification in 47cases of the bursting thoracic-lumbar fractures, which were operated using the pedicle screws.
OBJECTIVE
To judge the effectiveness of posterior short segment instrumented fusion in thoracic-lumbar fractures according to the Load-Sharing classification. MATERIAL AND METHOD: From 1995 through 1998, 47 patients who had been operated with short segment transpedicular instrumentation including fractured vertebra were selected and they were divided two groups, one below 6 point of Load-Sharing score, the other above 7 point. In follow up of average 39 months, the guide of reduction loss, which include the change of anterior vertebral body height and sagittal index were analysed statistically with the Student T-test at the postoperative time and the last follow-up time.
RESULTS
In group below 6 point, the average of anterior vertebral body height was 56.2% before the operation and reduced 77.6% after the operation and measured 76.4% at final follow-up. The reduction loss was 1.2%. The sagittal index of preoperative 19.4degree became 10.6degree after the operation and measured 11.8degree at the last follow-up. The loss of correction angle was 1.2degree . In the other group above 7 point, anterior vertebral body height was average 51.7% before the operation and reduced 75% after the operation and measured 71.2% in last follow up, so reduction loss was 3.8%. Sagittal index was average 21.6degree before the operation and corrected 12.6 after the operation and measured 14.6degree in last follow up. All of 19 patients with neurologic deficits improved by over the one Frankel grade except grade A.
CONCLUSION
Although the additional study is needed, there were no significant difference of statistical analysis about indexes between two groups.
Keyword
MeSH Terms
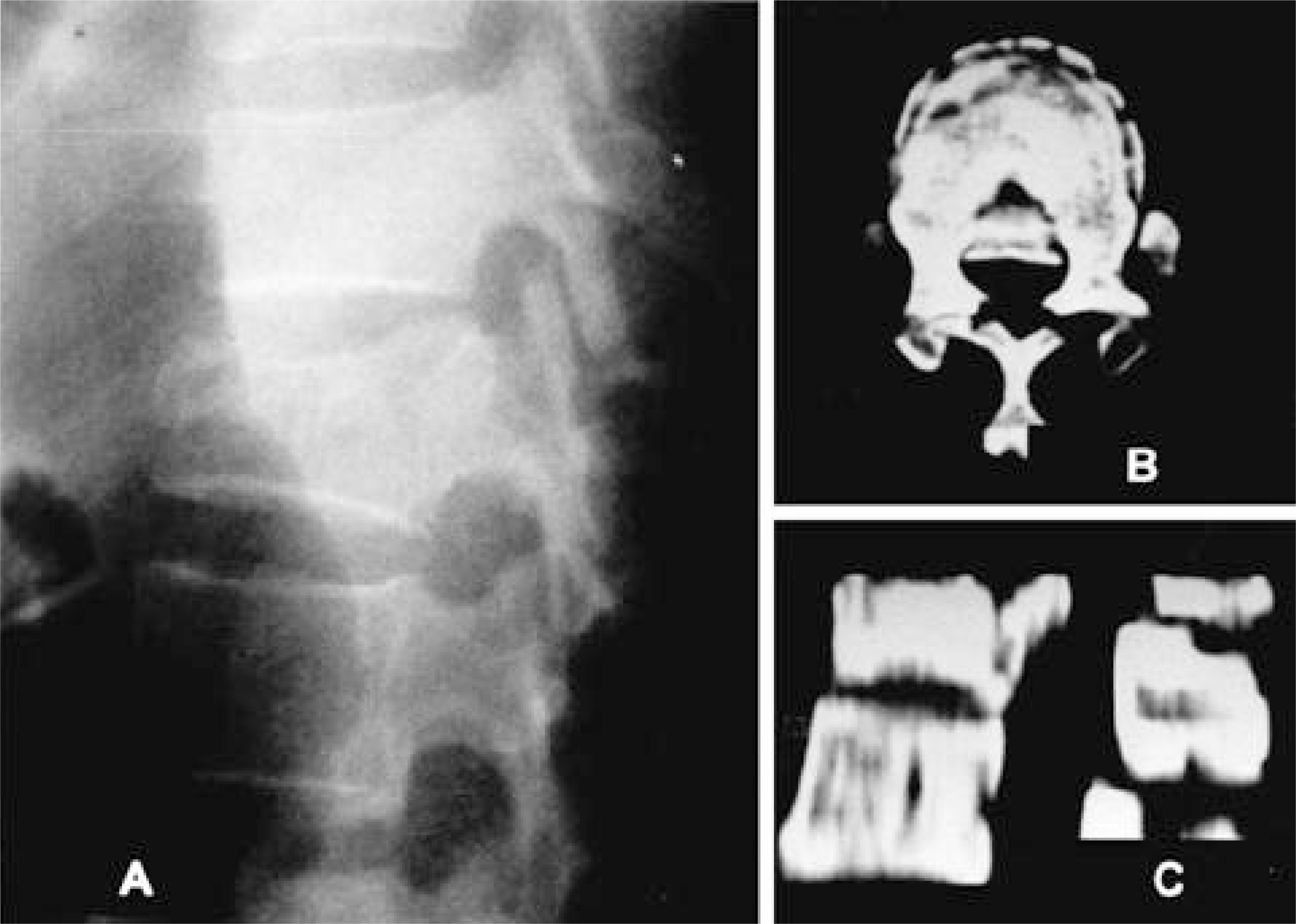
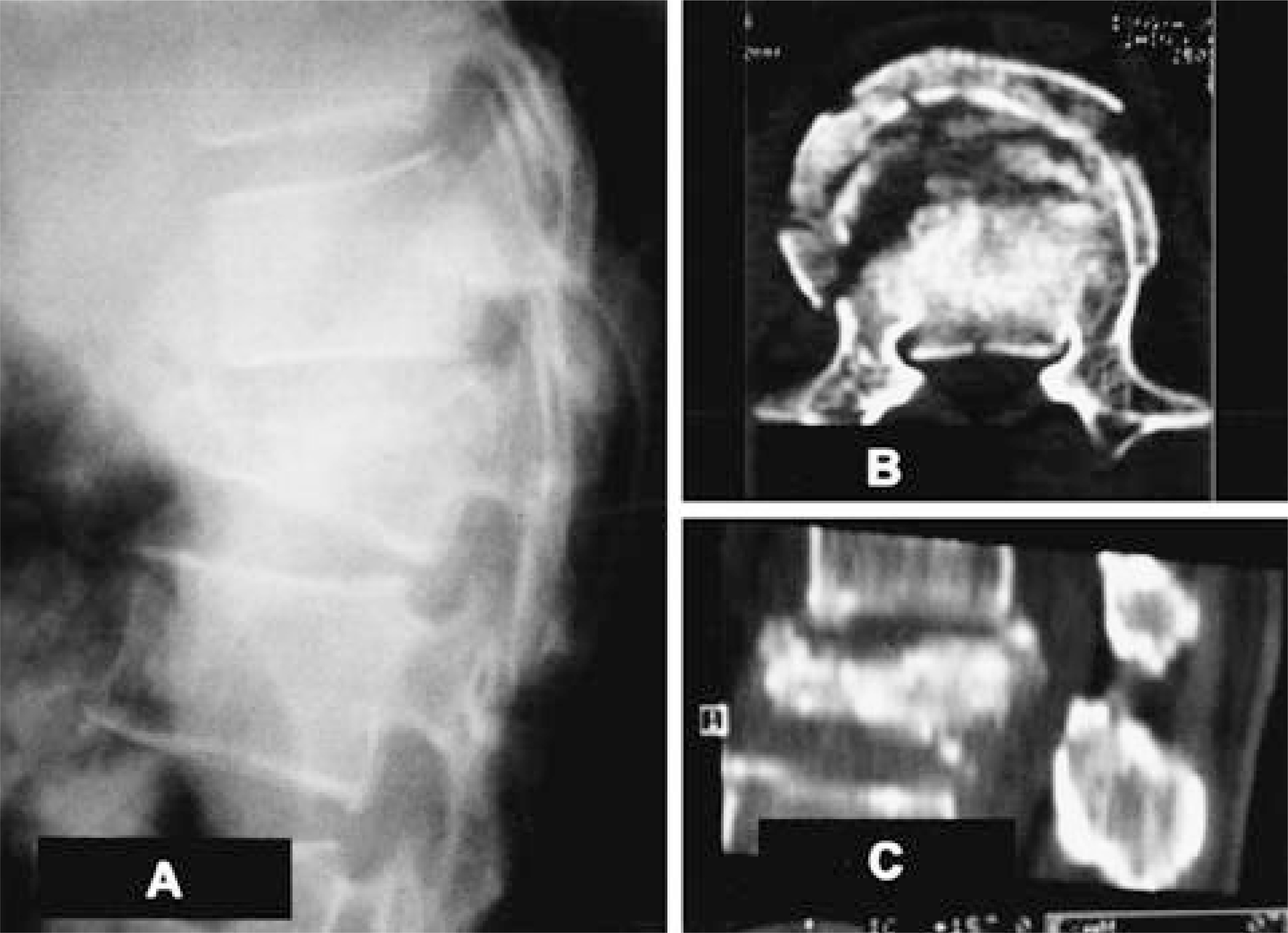
Figure
Reference
-
1). Bernhardt M, Bridwell KH. Segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and thoracolumbar junction, spine. 14:717. 1989.2). Carl AL, Tromanhauser SG, Roger DJ. Pedicle screw instrumentation for thoracolumbar burst fractures and fracture-dislocation. Spine. 17:S317–S324. 1992.3). Chung JY, Rhym IS. Short segment transpedicular Cotrel-Dubousset instrumentation including involved vertebra for fractures of thoracic and lumbar spine. J Korean Orthop Assoc. 29(3):940–948. 1994.
Article4). Frankel HL, Hancock DO, Hyslop G, Melzak J, Michae-lis LS, Ungar GH, Vernon JDS, Walsh JJ. The Value of Postural Reduction in the Initial Management of Closed Injuries of the Spine with Paraplegia and Tetraplegia Pant I. Paraplegia. 7:179–192. 1969.5). Gurr KR, McAfee PC. Biomechanical analysis of anterior and posterior instrumentation systems after cor -pectomy: A calf-spine model. J Bone Joint Surg. 70A:1182–1191. 1988.6). Jeong ST, Cho SH, Song HR, Koo KH, Park HB, Chung UH. Comparison of short and long - segment fusion in thoracic and lumbar fracture. J Korean Spine Surg. 6(1):73–80. 1999.7). Lee CS, Chung SS, Jung HW, Kim ES. Decision of posterior fixation level by load-sharing classification in thoracolumbar and lumbar bursting fracture. J Korean Spine Surg. 8(1):27–38. 2001.8). McAfee PC, Weiland DJ, Carlow JJ. Survivorship analysis of pedicle spinal instrumentation. Spine. 16(sup -plement 8):422–427. 1991.
Article9). McCormack T, Karaikoric E, Gaines RW. The Load Sharing Classification of Spine Fractures, Spine. 19:1741–1744. 1994.10). McLain RF, Sparling E, Benson DR. Early Failure of Short-Segment Pedicle Instrumentation for Thoracolumbar Fractures. J Bone Joint Surg. 75-A:162–167. 1993.11). McNamara MJ, Stephens GC, Spengler DM. Tr ans-pedicular Short Segment Fusion for Treatment of Lumbar Burst Fractures. J Spinal Disord. 5:183–187. 1992.12). Parker JW, Lone JR, Karaikoric EE, Gaines RW. Successful Short-Segment Instrumentation and Fusion for Thoracolumber Spine Fractures. Spine. 25:1157–1169. 2000.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Posterior Short-Segment Instrumentation of Thoracic and Lumbar Bursting Fractures: Retrospective study related with Load-Sharing classification
- Treatment of Thoraco-Lumbar Bursting Fractures According to Load-Sharing Classification
- Comparison of Short Segment and Long Segment Posterior Instrumentation of Thoracolumbar and Lumbar Bursting Fractures at Load Sharing Score 7 or Above
- The Outcomes of Short and Long Segment Posterior Instrumentation of Thoracolumbar Burst Fractures with a Load Sharing Score of 7 or More
- Decision of Posterior Fixation Level by Load-Sharing Classification in Thoracolumbar and Lumbar Burst Fracture