J Korean Soc Spine Surg.
2001 Sep;8(3):259-263. 10.4184/jkss.2001.8.3.259.
Pre-sacral Giant Schwannoma: Removal by a Combined Anterior and Posterior Approach: A Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Soonchunhyang University, Seoul, Korea. Korea junghowon@zaigen.co.kr
- 2Department of Clinical Pathology, College of Medicine, Soonchunhyang University, Seoul, Korea.
- KMID: 2209744
- DOI: http://doi.org/10.4184/jkss.2001.8.3.259
Abstract
-
STUDY DESIGN: This case report presents a rare case of pre-sacral giant schwannoma which originates from the S1 nerve root.
OBJECTIVES
To discuss a surgical approach for removal of pre-sacral giant schwannoma and review the pertinent literatures. SUMMARY OF LITERATURE REVIEW: Pre-sacral tumors are unusual neoplasms that cause approximately one in 40,000 hospital admissions. Schwannoma represents only a small fraction of the many types of tumors that may be present in this region. Less than 1% of all spinal schwannomas occur in the sacrum. The treatment of this lesion is complete removal, which is curative.
MATERIALS AND METHODS
A 46-year-old woman developed gradual back pain and radiating pain on her left lower extremity for about a year. There was no noted improvement with the use of conservative treatment. T1-weighted sagittal MRI reveals a large homogeneous low-signal intensity mass on left pre-sacral area and intrasacral extension of the tumor forming a dumbbell shaped mass.
RESULTS
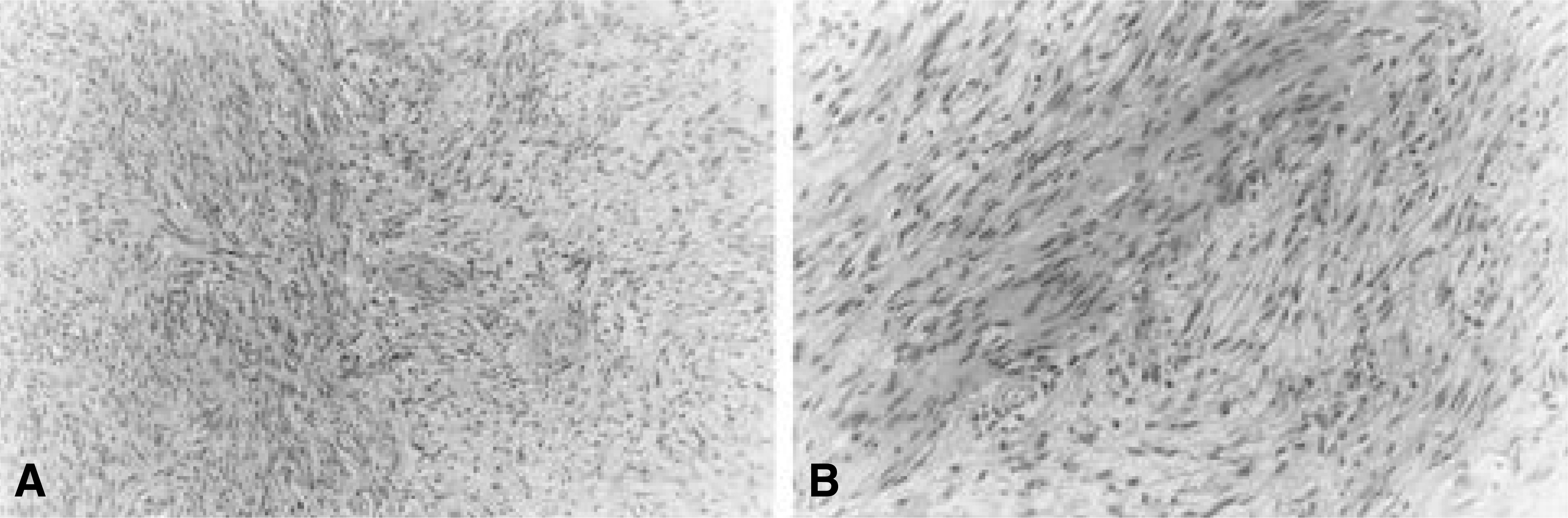
The tumor was completely removed by a combined anterior and posterior approach. The excised mass was cylindrical, measuring 8x4x3cm in size, which had originated from the S1 nerve root. It was histologically diagnosed as benign schwannoma. Satisfactory result was obtained after the complete removal of the mass.
CONCLUSIONS
We report a case of the successful and complete removal of a pre-sacral giant schwannoma and the affected nerve root through a combined anterior and posterior approach.
MeSH Terms
Figure
Reference
-
1). Abernathey CD, Onofrio BM, Scheithauer B, Pairolero PC, Shives TC. Surgical management of giant sacral schwannomas. J Neurosurg. 65:286–295. 1986.
Article2). Acciarri N, Staffa G, Poppi M. Giant sacral schwannoma: removal by anterior, transabdominal approach. Br J Neurosurg. 10(5):489–492. Oct. 1996.3). Das Gupta TK, Brasfield RD, Strong EW, Hajolu SI. Benign solitary schwannomas. Cancer. 24(2):355–366. Aug. 1969.4). Gupta S, Sikora SS, Gupta R, Singh MK, Chatto-padhyay TK. Presacral neurilemoma(schwannoma): Report of a rare case. Jpn J Surg. 19(2):229–231. 1989.5). Kim P, Ebersold MJ, Onofrio BM, Quast LM. Surgery of spinal nerve schwannoma. Risk of neurological deficit after resection of involved root. J Neurosurg. 71:810–814. 1989.6). Madanes A, Ucci A, Mitchell GW Jr. Presacral neu-rilemmoma. A case report and literature review. J Reprod Med. 27(6):356–358. Jun. 1982.7). Rengachary SS, O'Boynick P, Batnitzky S, Kepes JJ. Giant intrasacral schwannoma: Case report. Neurosurgery. 9(5):573–577. Nov. 1981.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pre-sacral Giant Schwannoma: Removal by a Combined Anterior and Posterior Approach: A Case Report
- Giant Benign Schwannoma Involving Sacral Bone
- Single Stage Posterior Approach for Total Resection of Presacral Giant Schwannoma: A Technical Case Report
- An Extremely Giant Lumbar Schwannoma: New Classification (Kotil) and Mini-Open Microsurgical Resection
- Cystic Giant Sacral Schwannoma Mimicking Aneurysmal Bone Cyst : A Case Report and Review of Literatures