Yonsei Med J.
2012 Jul;53(4):723-728. 10.3349/ymj.2012.53.4.723.
Recurrent Varicoceles: Causes and Treatment Using Angiography and Magnification Assisted Subinguinal Varicocelectomy
- Affiliations
-
- 1Department of Urology, University of Ulsan College of Medicine, Ulsan University Hospital, Ulsan, Korea. scpark@amc.seoul.kr
- 2Department of Anesthesiology and Pain Medicine, Jeju National University College of Medicine, Jeju National Universtiy Hospital, Jeju, Korea.
- 3Department of Urology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- 4School of Mechanical Engineering, Pusan National University, Busan, Korea.
- KMID: 1716869
- DOI: http://doi.org/10.3349/ymj.2012.53.4.723
Abstract
- PURPOSE
To investigate the causes of varicocele recurrence and assess the use of embolization and subinguinal varicocelectomy in its treatment in patients with angiography and subinguinal varicocelectomy.
MATERIALS AND METHODS
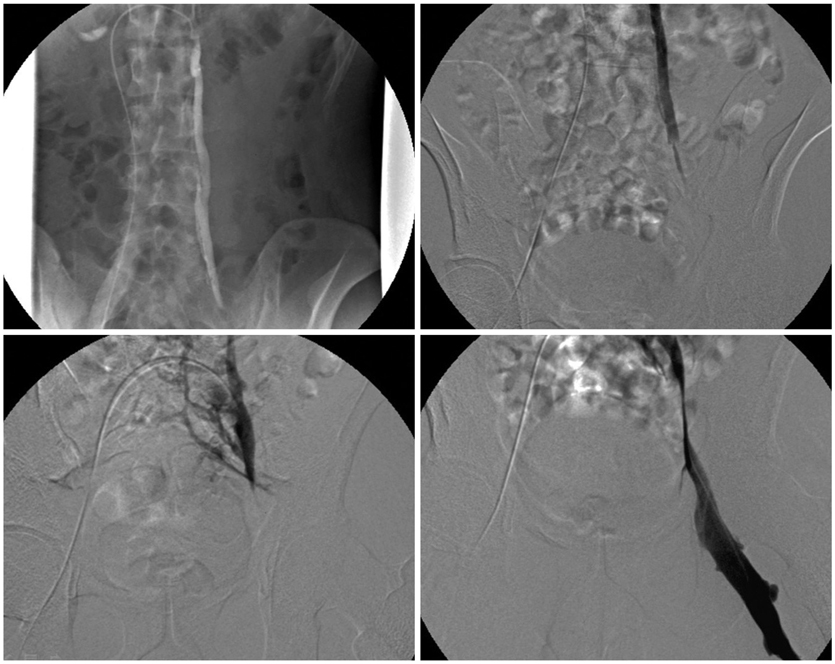
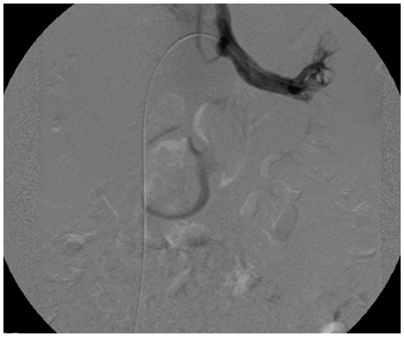
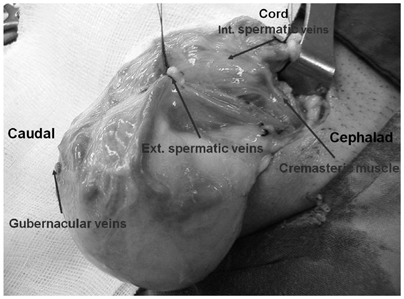
The present study involved 15 patients with recurrent varicoceles. The mean patient age was 21.2 years (range: 12-42 years). Preoperative angiography was performed in 11 patients. Embolization was used in patients with patent internal spermatic veins (ISVs). Patients without patent ISVs or preoperative angiography underwent magnification-assisted subinguinal varicocelectomy which included testicular retrieval and ligation of all collateral veins except arteries and deferential veins.
RESULTS
Seven among 11 patients (64%) which had preoperative angiography had patent ISVs and underwent embolization and 8 patients underwent subinguinal varicocelectomy. Of those 8 patients, 6 had dilated ISVs and external spermatic veins (ESVs), one had dilated ISVs and gubernacular veins, and one had dilated ISVs, ESVs and gubernacular veins. No patient experienced recurrence or testis atrophy.
CONCLUSION
Patent ISVs or collateral veins may be the cause of recurrence after varicocelectomy. Angiographic embolization was successful in 64% of recurrent varicoceles patients with patent ISVs. However, microscope-assisted subinguinal varicocelectomy may be the best overall treatment for patients with recurrent varicoceles.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Magnification-Assisted Subinguinal Varicocelectomy with Testicular Delivery in Children: A Preliminary Report
Suk Ju Cho, Seong Cheol Kim, Kun Suk Kim, Sungchan Park
World J Mens Health. 2014;32(2):93-98. doi: 10.5534/wjmh.2014.32.2.93.
Reference
-
1. Naughton CK, Nangia AK, Agarwal A. Pathophysiology of varicoceles in male infertility. Hum Reprod Update. 2001. 7:473–481.2. Beck EM, Schlegel PN, Goldstein M. Intraoperative varicocele anatomy: a macroscopic and microscopic study. J Urol. 1992. 148:1190–1194.
Article3. Goldstein M, Gilbert BR, Dicker AP, Dwosh J, Gnecco C. Microsurgical inguinal varicocelectomy with delivery of the testis: an artery and lymphatic sparing technique. J Urol. 1992. 148:1808–1811.
Article4. Lee JW, Paick JS, Kim SW. Microsurgical subinguinal varicocelectomy: comparison of pediatric and adult patients. Korean J Urol. 2008. 49:1029–1034.
Article5. Al-Kandari AM, Shabaan H, Ibrahim HM, Elshebiny YH, Shokeir AA. Comparison of outcomes of different varicocelectomy techniques: open inguinal, laparoscopic, and subinguinal microscopic varicocelectomy: a randomized clinical trial. Urology. 2007. 69:417–420.
Article6. Franco G, Iori F, de Dominicis C, Dal Forno S, Mander A, Laurenti C. Challenging the role of cremasteric reflux in the pathogenesis of varicocele using a new venographic approach. J Urol. 1999. 161:117–121.
Article7. Franco G, Leonardo C. Is selective internal spermatic venography necessary in detecting recurrent varicocele after surgical repair? Eur Urol. 2002. 42:192–193.
Article8. Dubin L, Amelar RD. Varicocele size and results of varicocelectomy in selected subfertile men with varicocele. Fertil Steril. 1970. 21:606–609.
Article9. Lord DJ, Burrows PE. Pediatric varicocele embolization. Tech Vasc Interv Radiol. 2003. 6:169–175.
Article10. Cayan S, Shavakhabov S, Kadioğlu A. Treatment of palpable varicocele in infertile men: a meta-analysis to define the best technique. J Androl. 2009. 30:33–40.
Article11. Al-Said S, Al-Naimi A, Al-Ansari A, Younis N, Shamsodini A, A-sadiq K, et al. Varicocelectomy for male infertility: a comparative study of open, laparoscopic and microsurgical approaches. J Urol. 2008. 180:266–270.
Article12. Murray RR Jr, Mitchell SE, Kadir S, Kaufman SL, Chang R, Kinnison ML, et al. Comparison of recurrent varicocele anatomy following surgery and percutaneous balloon occlusion. J Urol. 1986. 135:286–289.
Article13. Kaufman SL, Kadir S, Barth KH, Smyth JW, Walsh PC, White RI Jr. Mechanisms of recurrent varicocele after balloon occlusion or surgical ligation of the internal spermatic vein. Radiology. 1983. 147:435–440.
Article14. Sze DY, Kao JS, Frisoli JK, McCallum SW, Kennedy WA 2nd, Razavi MK. Persistent and recurrent postsurgical varicoceles: venographic anatomy and treatment with N-butyl cyanoacrylate embolization. J Vasc Interv Radiol. 2008. 19:539–545.
Article15. Abdel-Maguid AF, Othman I. Microsurgical and nonmagnified subinguinal varicocelectomy for infertile men: a comparative study. Fertil Steril. 2010. 94:2600–2603.
Article16. Rais-Bahrami S, Montag S, George AK, Rastinehad AR, Palmer LS, Siegel DN. Angiographic Findings of Primary Versus Salvage Varicoceles Treated with Selective Gonadal Vein Embolization: An Explanation for Surgical Treatment Failure. J Endourol. 2012. [Epub ahead of print].
Article17. Feneley MR, Pal MK, Nockler IB, Hendry WF. Retrograde embolization and causes of failure in the primary treatment of varicocele. Br J Urol. 1997. 80:642–646.
Article18. Coolsaet BL. The varicocele syndrome: venography determining the optimal level for surgical management. J Urol. 1980. 124:833–839.
Article19. Bähren W, Lenz M, Porst H, Wierschin W. Side effects, complications and contraindications for percutaneous sclerotherapy of the internal spermatic vein in the treatment of idiopathic varicocele. Rofo. 1983. 138:172–179.
Article20. Libman JL, Segal R, Baazeem A, Boman J, Zini A. Microanatomy of the left and right spermatic cords at subinguinal microsurgical varicocelectomy: comparative study of primary and redo repairs. Urology. 2010. 75:1324–1327.
Article21. Grober ED, Chan PT, Zini A, Goldstein M. Microsurgical treatment of persistent or recurrent varicocele. Fertil Steril. 2004. 82:718–722.
Article22. Punekar SV, Prem AR, Ridhorkar VR, Deshmukh HL, Kelkar AR. Post-surgical recurrent varicocele: efficacy of internal spermatic venography and steel-coil embolization. Br J Urol. 1996. 77:124–128.
Article23. Kim J, Shin JH, Yoon HK, Ko GY, Gwon DI, Kim EY, et al. Persistent or recurrent varicocoele after failed varicocoelectomy: outcome in patients treated using percutaneous transcatheter embolization. Clin Radiol. 2012. 67:359–365.
Article24. Nabi G, Asterlings S, Greene DR, Marsh RL. Percutaneous embolization of varicoceles: outcomes and correlation of semen improvement with pregnancy. Urology. 2004. 63:359–363.
Article25. Storm DW, Hogan MJ, Jayanthi VR. Initial experience with percutaneous selective embolization: a truly minimally invasive treatment of the adolescent varicocele with no risk of hydrocele development. J Pediatr Urol. 2010. 6:567–571.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recurrent Varicoceles: Causes and Treatment Using Angiography and Magnification Assisted Subinguinal Varicocelectomy
- Clinical Outcomes of Varicocele Repair in Infertile Men: A Review
- Microsurgical Subinguinal Varicocelectomy: Comparison of Pediatric and Adult Patients
- Comparison of Laparosopic Varicocelectomy with Subinguinal Varicocelectomy
- Varicocele and male infertility