Yonsei Med J.
2009 Apr;50(2):284-288.
A Case of Cerebral Gumma Presenting as Brain Tumor in a Human Immunodeficiency Virus (HIV)-Negative Patient
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, Inha University, Incheon, Korea. ljinsoo@medimail.co.kr
- 2Department of Pathology, College of Medicine, Inha University, Incheon, Korea.
- 3Department of Radiology, College of Medicine, Inha University, Incheon, Korea.
- 4Department of Internal Medicine, Daesung General Hospital, Incheon, Korea.
- 5Department of Neurosuergery, Yonsei University Hospital, Seoul, Korea.
Abstract
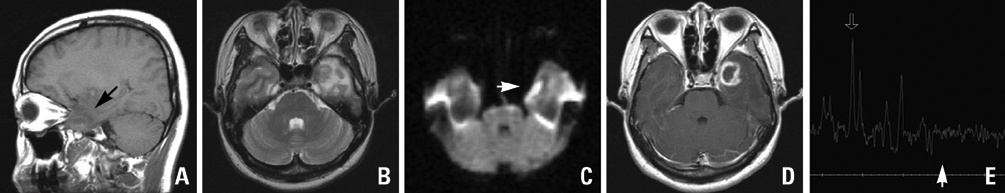
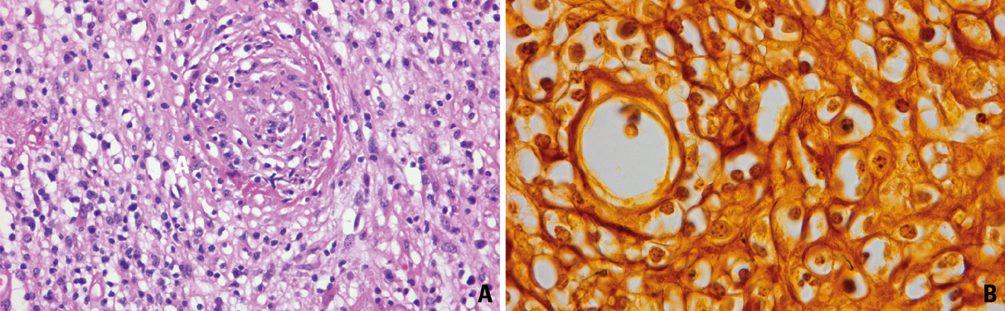
- Syphilis, along with the recent increase of human immunodeficiency virus (HIV) patients, has also been on the rise. It has a broad spectrum of clinical manifestations, among which cerebral gumma is, a kind of neurosyphilis, however, it is rare and can be cured by penicillin. Thus, cerebral gumma needs to be differentially diagnosed from other brain masses that may be present in syphilis patients. We have experienced a case where the patient was first suspected of brain tumor, but confirmed by surgery to be cerebral gumma due to neurosyphilis. This is the first such case encountered in Korea, therefore, we report it here in. A 40-year old woman complaining of headaches was found to have a brain mass on her CT scans and MRI. Suspecting a brain Tumor, a resection was performed on the patient, and histological results revealed that the central portion of the mass contained necrotic material and the peripheral region was infiltrated with plasma cells. Warthin-Starry staining of the region revealed spirochetes, and the patient was thus diagnosed as brain gumma. Venereal Disease Research Laboratory (VDRL) of cerebrospinal fluid (CSF) was reactive. After an operation, penicillin-G at a daily dose of 24x10(6) U was given for 10 days from post-operative day 10, and thereafter, the mass disappeared.
MeSH Terms
Figure
Reference
-
1. Hook EW 3rd, Marra CM. Acquired syphilis in adults. N Engl J Med. 1992. 326:1060–1069.
Article2. Wolters EC. Treatment of neurosyphilis. Clin Neuropharmacol. 1987. 10:143–154.
Article3. Ances BM, Danish SF, Kolson DL, Judy KD, Liebeskind DS. Cerebral gumma mimicking glioblastoma multiforme. Neurocrit Care. 2005. 2:300–302.
Article4. Pall HS, Williams AC, Stockley RA. Intracranial gumma presenting as a cerebral tumour. J R Soc Med. 1988. 81:603–604.
Article5. Mitka M. US effort to eliminate syphilis moving forward. JAMA. 2000. 283:1555–1556.
Article6. Hopkins RS, Jajosky RA, Hall PA, Adams DA, Connor FJ, Sharp P, et al. Summary of notifiable diseases--United States, 2003. MMWR Morb Mortal Wkly Rep. 2005. 52:1–85.7. Doherty L, Fenton KA, Jones J, Paine TC, Higgins SP, Williams D, et al. Syphilis: old problem, new strategy. BMJ. 2002. 325:153–156.
Article8. Jang HC, Cho JH, Park WB, Lee KD, Lee CS, Kim HB, et al. Outbreak of primary and secondary syphilis among HIV sero-positive patients in Korea. Infect Chemother. 2004. 36:366–372.9. Johns DR, Tierney M, Felsenstein D. Alteration in the natural history of neurosyphilis by concurrent infection with the human immuno deficiency virus. N Engl J Med. 1987. 316:1569–1572.
Article10. Clark EG, Danbolt N. The Oslo study of the natural history of untreated syphilis; an epidemiologic investigation based on a restudy of the Boeck-Bruusgaard material; a review and appraisal. J Chronic Dis. 1955. 2:311–344.11. Scheck DN, Hook EW 3rd. Neurosyphilis. Infect Dis Clin North Am. 1994. 8:769–795.
Article12. Merritt HH, Adams RD, Solomon HC. Neurosyphilis. 1946. New York: Oxford University Press;62–66.13. Berger JR, Waskin H, Pall L, Hensley G, Ihmedian I, Post MJ. Syphilitic cerebral gumma with HIV infection. Neurology. 1992. 42:1282–1287.
Article14. Horowitz HW, Valsamis MP, Wicher V, Abbruscato F, Larsen SA, Wormser GP, et al. Brief report: cerebral syphilitic gumma confirmed by the polymerase chain reaction in a man with human immunodeficiency virus infection. N Engl J Med. 1994. 331:1488–1491.
Article15. Agrons GA, Han SS, Husson MA, Simeone F. MR imaging of cerebral gumma. AJNR Am J Neuroradiol. 1991. 12:80–81.16. Vogl T, Dresel S, Lochmüller H, Bergman C, Reimers C, Lissner J. Third cranial nerve palsy caused by gummatous neurosyphilis: MR findings. AJNR Am J Neuroradiol. 1993. 14:1329–1331.17. Brightbill TC, Ihmeidan IH, Post MJ, Berger JR, Katz DA. Neurosyphilis in HIV-positive and HIV-negative patients: neuroimaging findings. AJNR Am J Neuroradiol. 1995. 16:703–711.18. Cartes-Zumelzu FW, Stavrou I, Castillo M, Eisenhuber E, Knosp E, Thurnher MM. Diffusion-weighted imaging in the assessment of brain abscesses therapy. AJNR Am J Neuroradiol. 2004. 25:1310–1317.19. Suarez JI, Mlakar D, Snodgrass SM. Cerebral syphilitic gumma in an HIV-negative patient presenting as prolonged focal motor status epilepticus. N Engl J Med. 1996. 335:1159–1160.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cerebral Gumma Mimicking a Brain Tumor in a Human Immunodeficiency Virus-Negative Patient: A Case Report
- A Case of Cerebral Gumma Presenting as Brain Tumor in a Human Immunodeficiency Virus (HIV)-Negative Patient
- Cerebral Syphilitic Gumma Mimicking a Brain Tumor in the Relapse of Secondary Syphilis in a Human Immunodeficiency Virus-Negative Patient
- Primary Effusion Lymphoma in a Non-Human Immunodeficiency Virus Patient: A Case Report
- Human Immunodeficiency Virus-Associated Multiple Cerebral Aneurysmal Vasculopathy in a Young Adult: A Case Report