Comparison of the Diagnostic Accuracies of 1.5T and 3T Stress Myocardial Perfusion Cardiovascular Magnetic Resonance for Detecting Significant Coronary Artery Disease
- Affiliations
-
- 1Department of Radiology, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul 05030, Korea. ksm9723@yahoo.co.kr
- 2Department of Cardiology, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul 05030, Korea.
- 3Department of Thoracic Surgery, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul 05030, Korea.
- KMID: 2424841
- DOI: http://doi.org/10.3348/kjr.2018.19.6.1007
Abstract
OBJECTIVE
To compare the diagnostic performance of cardiovascular magnetic resonance (CMR) myocardial perfusion at 1.5- and 3-tesla (T) for detecting significant coronary artery disease (CAD), with invasive coronary angiography (ICA) as the reference method.
MATERIALS AND METHODS
We prospectively enrolled 281 patients (age 62.4 ± 8.3 years, 193 men) with suspected or known CAD who had undergone 1.5T or 3T CMR and ICA. Two independent radiologists interpreted perfusion defects. With ICA as the reference standard, the diagnostic performance of 1.5T and 3T CMR for identifying significant CAD (≥ 50% diameter reduction of the left main and ≥ 70% diameter reduction of other epicardial arteries) was determined.
RESULTS
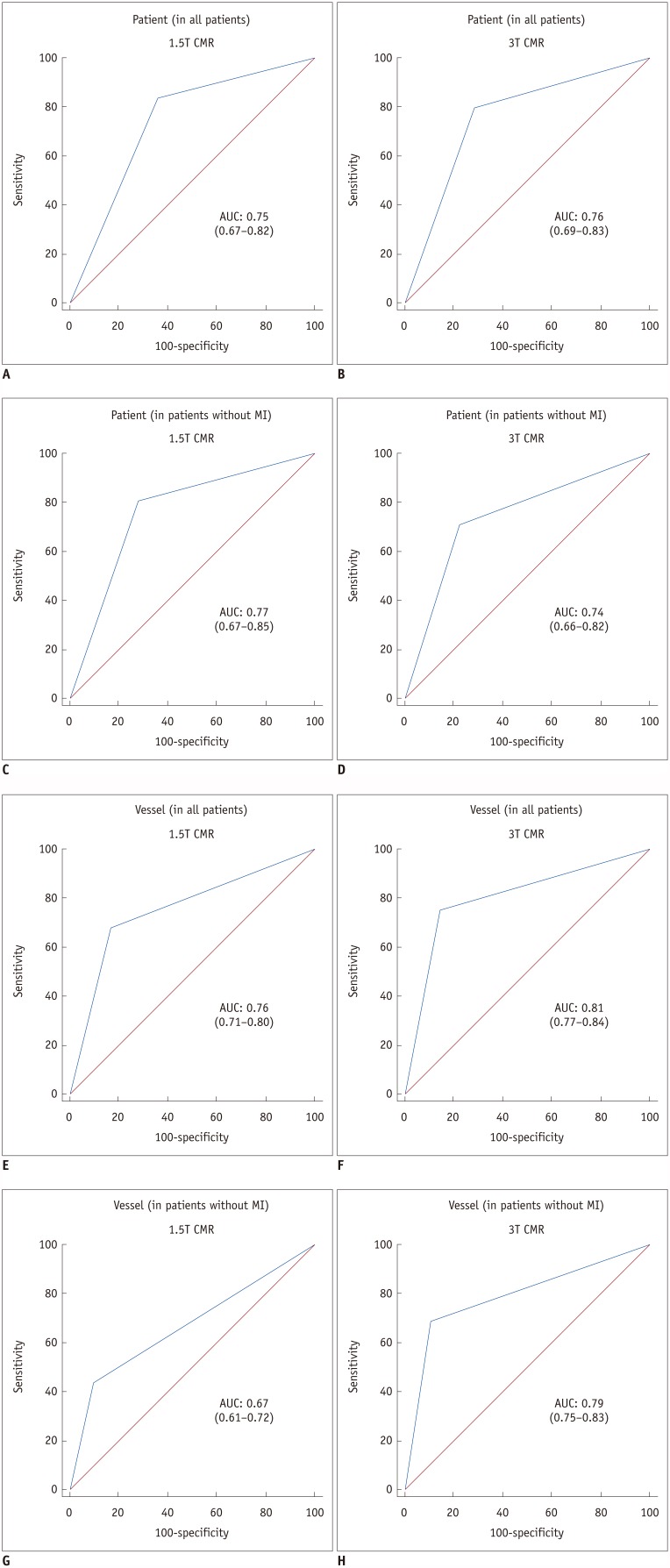
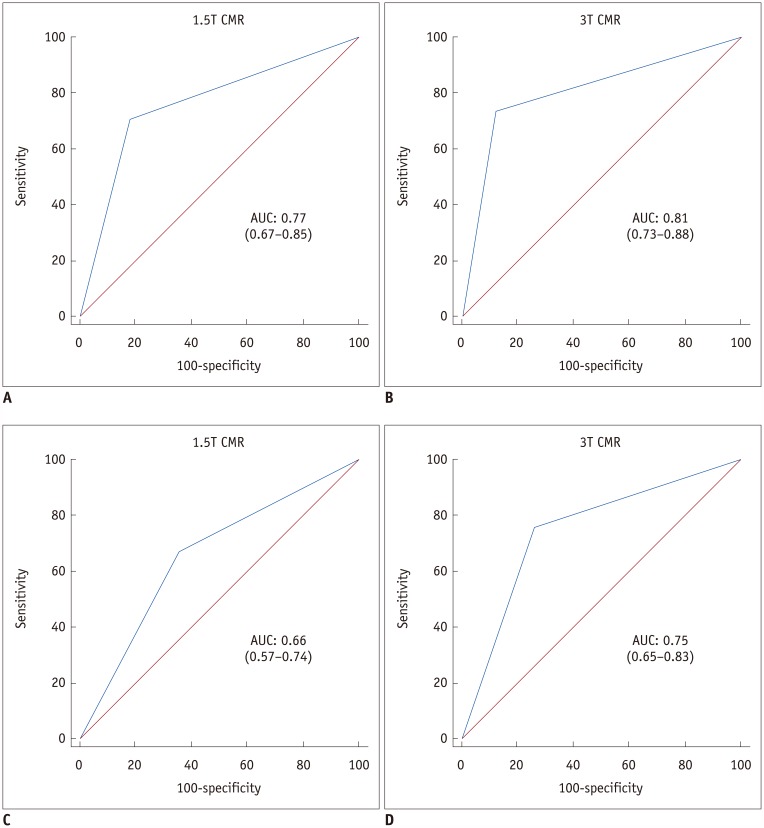
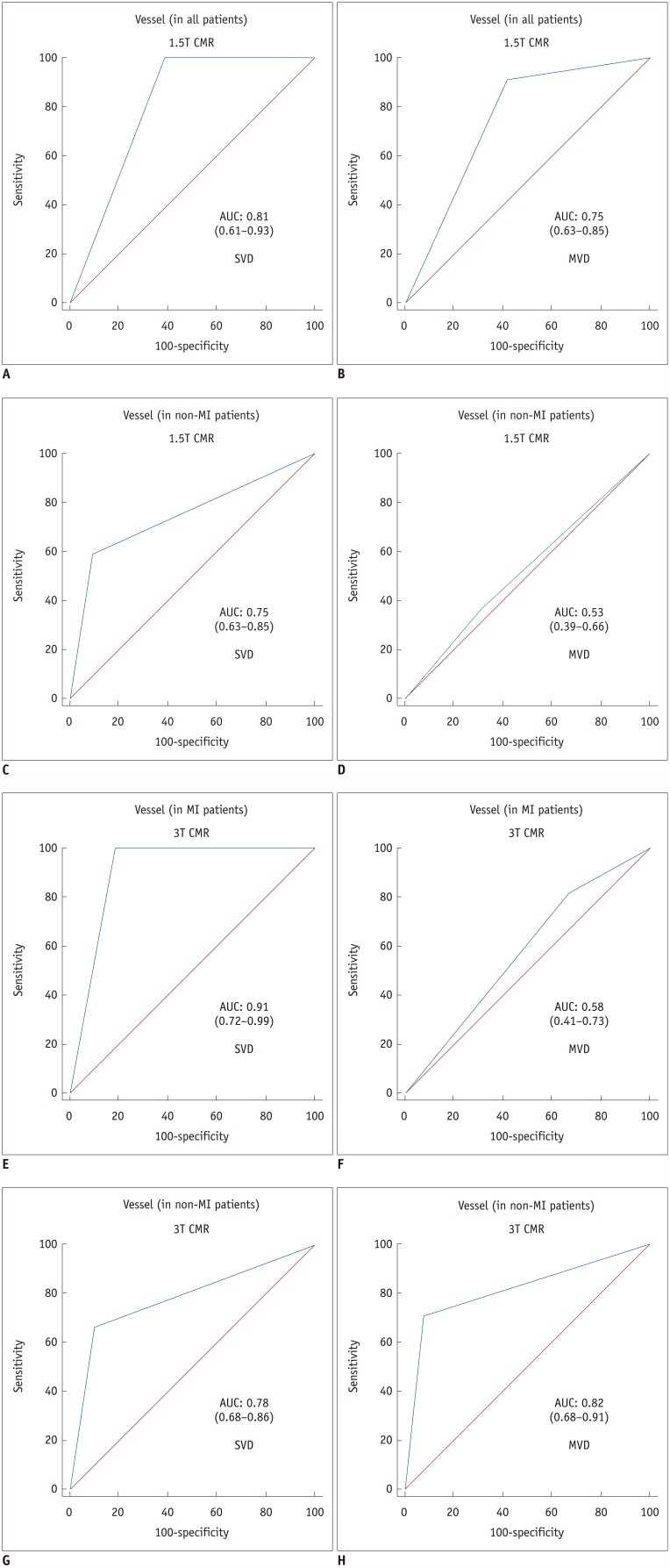
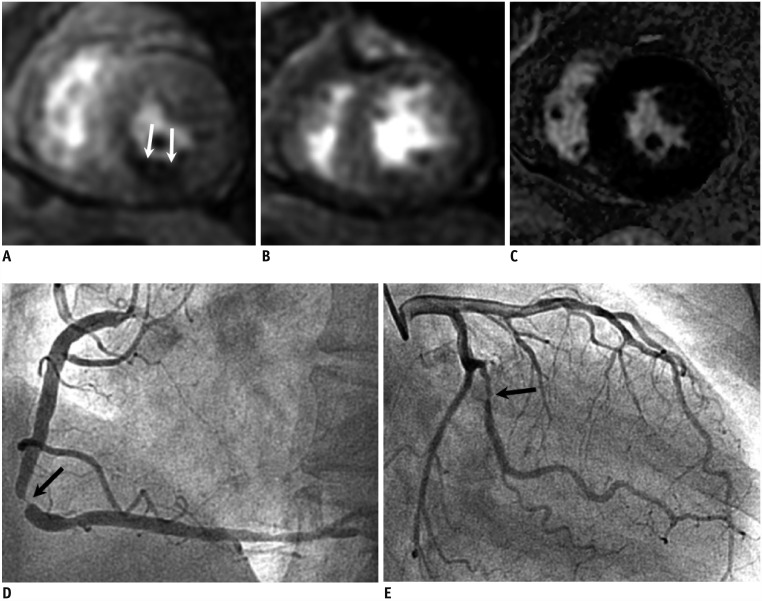
No differences were observed in baseline characteristics or prevalence of CAD and old myocardial infarction (MI) using 1.5T (n = 135) or 3T (n = 146) systems. Sensitivity, specificity, positive and negative predictive values, and area under the receiver operating characteristic curve (AUC) for detecting significant CAD were similar between the 1.5T (84%, 64%, 74%, 76%, and 0.75 per patient and 68%, 83%, 66%, 84%, and 0.76 per vessel) and 3T (80%, 71%, 71%, 80%, and 0.76 per patient and 75%, 86%, 64%, 91%, and 0.81 per vessel) systems. In patients with multi-vessel CAD without old MI, the sensitivity, specificity, and AUC with 3T were greater than those with 1.5T on a per-vessel basis (71% vs. 36%, 92% vs. 69%, and 0.82 vs. 0.53, respectively).
CONCLUSION
3T CMR has similar diagnostic performance to 1.5T CMR in detecting significant CAD, except for higher diagnostic performance in patients with multi-vessel CAD without old MI.
Keyword
MeSH Terms
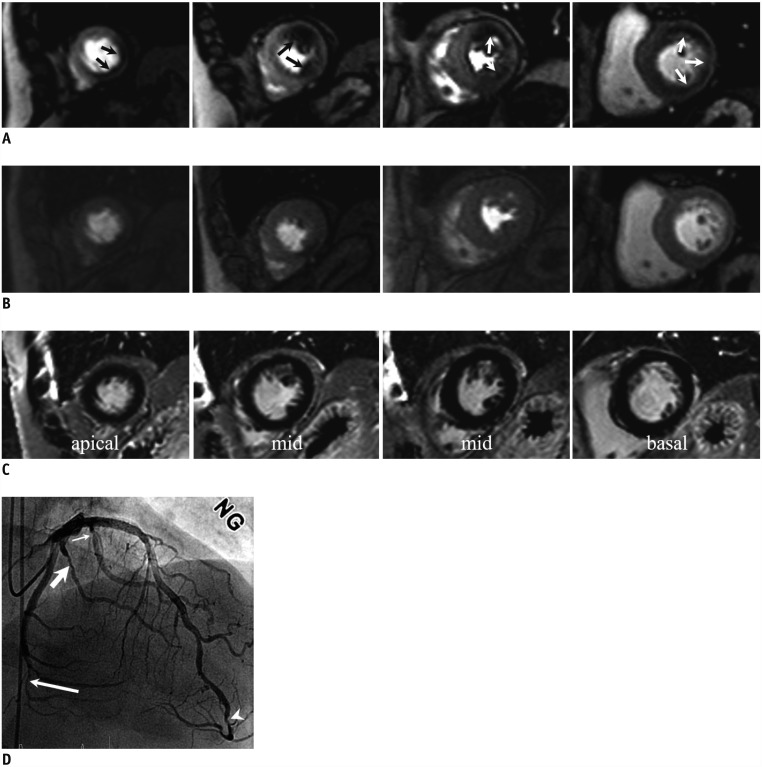
Figure
Cited by 5 articles
-
Guidelines for Cardiovascular Magnetic Resonance Imaging from the Korean Society of Cardiovascular Imaging—Part 2: Interpretation of Cine, Flow, and Angiography Data
Jae Wook Lee, Jee Hye Hur, Dong Hyun Yang, Bae Young Lee, Dong Jin Im, Su Jin Hong, Eun Young Kim, Eun-Ah Park, Yeseul Jo, JeongJae Kim, Chul Hwan Park, Hwan Seok Yong
Korean J Radiol. 2019;20(11):1477-1490. doi: 10.3348/kjr.2019.0407.Guideline for Cardiovascular Magnetic Resonance Imaging from the Korean Society of Cardiovascular Imaging—Part 1: Standardized Protocol
Yeseul Jo, JeongJae Kim, Chul Hwan Park, Jae Wook Lee, Jee Hye Hur, Dong Hyun Yang, Bae Young Lee, Dong Jin Im, Su Jin Hong, Eun Young Kim, Eun-Ah Park, Pan Ki Kim, Hwan Seok Yong
Korean J Radiol. 2019;20(9):1313-1333. doi: 10.3348/kjr.2019.0398.Guidelines for Cardiovascular Magnetic Resonance Imaging from the Korean Society of Cardiovascular Imaging—Part 3: Perfusion, Delayed Enhancement, and T1- and T2 Mapping
Dong Jin Im, Su Jin Hong, Eun-Ah Park, Eun Young Kim, Yeseul Jo, JeongJae Kim, Chul Hwan Park, Hwan Seok Yong, Jae Wook Lee, Jee Hye Hur, Dong Hyun Yang, Bae Young Lee
Korean J Radiol. 2019;20(12):1562-1582. doi: 10.3348/kjr.2019.0411.Myocardial Blood Flow Quantified by Low-Dose Dynamic CT Myocardial Perfusion Imaging Is Associated with Peak Troponin Level and Impaired Left Ventricle Function in Patients with ST-Elevated Myocardial Infarction
Jingwei Pan, Mingyuan Yuan, Mengmeng Yu, Yajie Gao, Chengxing Shen, Yining Wang, Bin Lu, Jiayin Zhang
Korean J Radiol. 2019;20(5):709-718. doi: 10.3348/kjr.2018.0729.Guidelines for Cardiovascular Magnetic Resonance Imaging from the Korean Society of Cardiovascular Imaging (KOSCI) - Part 3: Perfusion, Delayed Enhancement, and T1- and T2 Mapping
Dong Jin Im, Su Jin Hong, Eun-Ah Park, Eun Young Kim, Yeseul Jo, Jeong Jae Kim, Chul Hwan Park, Hwan Seok Yong, Jae Wook Lee, Jee Hye Hur, Dong Hyun Yang, Bae-Young Lee
Investig Magn Reson Imaging. 2020;24(1):1-20. doi: 10.13104/imri.2020.24.1.1.
Reference
-
1. ASCI Practice Guideline Working Group. Beck KS, Kim JA, Choe YH, Hian SK, Hoe J, et al. 2017 multimodality appropriate use criteria for noninvasive cardiac imaging: expert consensus of the Asian Society of Cardiovascular Imaging. Korean J Radiol. 2017; 18:871–880. PMID: 29089819.
Article2. Takx RA, Blomberg BA, El Aidi H, Habets J, de Jong PA, Nagel E, et al. Diagnostic accuracy of stress myocardial perfusion imaging compared to invasive coronary angiography with fractional flow reserve meta-analysis. Circ Cardiovasc Imaging. 2015; 8:pii: e002666.
Article3. Rieber J, Huber A, Erhard I, Mueller S, Schweyer M, Koenig A, et al. Cardiac magnetic resonance perfusion imaging for the functional assessment of coronary artery disease: a comparison with coronary angiography and fractional flow reserve. Eur Heart J. 2006; 27:1465–1471. PMID: 16720685.
Article4. Groothuis JG, Beek AM, Brinckman SL, Meijerink MR, van den Oever ML, Hofman MB, et al. Combined non-invasive functional and anatomical diagnostic work-up in clinical practice: the magnetic resonance and computed tomography in suspected coronary artery disease (MARCC) study. Eur Heart J. 2013; 34:1990–1998. PMID: 23475530.
Article5. Rajiah P, Bolen MA. Cardiovascular MR imaging at 3 T: opportunities, challenges, and solutions. Radiographics. 2014; 34:1612–1635. PMID: 25310420.
Article6. Meyer C, Strach K, Thomas D, Litt H, Nähle CP, Tiemann K, et al. High-resolution myocardial stress perfusion at 3 T in patients with suspected coronary artery disease. Eur Radiol. 2008; 18:226–233. PMID: 17851665.
Article7. Lockie T, Ishida M, Perera D, Chiribiri A, De Silva K, Kozerke S, et al. High-resolution magnetic resonance myocardial perfusion imaging at 3.0-Tesla to detect hemodynamically significant coronary stenoses as determined by fractional flow reserve. J Am Coll Cardiol. 2011; 57:70–77. PMID: 21185504.
Article8. Yun CH, Tsai JP, Tsai CT, Mok GS, Sun JY, Hung CL, et al. Qualitative and semi-quantitative evaluation of myocardium perfusion with 3 T stress cardiac MRI. BMC Cardiovasc Disord. 2015; 15:164. PMID: 26642757.
Article9. Strach K, Meyer C, Thomas D, Naehle CP, Schmitz C, Litt H, et al. High-resolution myocardial perfusion imaging at 3 T: comparison to 1.5 T in healthy volunteers. Eur Radiol. 2007; 17:1829–1835. PMID: 17429650.10. Walcher T, Ikuye K, Rottbauer W, Wöhrle J, Bernhardt P. Is contrast-enhanced cardiac magnetic resonance imaging at 3 T superior to 1.5 T for detection of coronary artery disease? Int J Cardiovasc Imaging. 2013; 29:355–361. PMID: 22825256.11. Cheng AS, Pegg TJ, Karamitsos TD, Searle N, Jerosch-Herold M, Choudhury RP, et al. Cardiovascular magnetic resonance perfusion imaging at 3-tesla for the detection of coronary artery disease: a comparison with 1.5-tesla. J Am Coll Cardiol. 2007; 49:2440–2244. PMID: 17599608.12. Jogiya R, Kozerke S, Morton G, De Silva K, Redwood S, Perera D, et al. Validation of dynamic 3-dimensional whole heart magnetic resonance myocardial perfusion imaging against fractional flow reserve for the detection of significant coronary artery disease. J Am Coll Cardiol. 2012; 60:756–765. PMID: 22818072.
Article13. Chung HW, Ko SM, Hwang HK, So Y, Yi JG, Lee EJ. Diagnostic performance of coronary CT angiography, stress dual-energy CT perfusion, and stress perfusion single-photon emission computed tomography for coronary artery disease: comparison with combined invasive coronary angiography and stress perfusion cardiac MRI. Korean J Radiol. 2017; 18:476–486. PMID: 28458600.
Article14. Ortiz-Pérez JT, Rodríguez J, Meyers SN, Lee DC, Davidson C, Wu E. Correspondence between the 17-segment model and coronary arterial anatomy using contrast-enhanced cardiac magnetic resonance imaging. JACC Cardiovasc Imaging. 2008; 1:282–293. PMID: 19356440.
Article15. Ebersberger U, Makowski MR, Schoepf UJ, Platz U, Schmidtler F, Rose J, et al. Magnetic resonance myocardial perfusion imaging at 3.0 Tesla for the identification of myocardial ischaemia: comparison with coronary catheter angiography and fractional flow reserve measurements. Eur Heart J Cardiovasc Imaging. 2013; 14:1174–1180. PMID: 23907345.
Article16. Mordini FE, Haddad T, Hsu LY, Kellman P, Lowrey TB, Aletras AH, et al. Diagnostic accuracy of stress perfusion CMR in comparison with quantitative coronary angiography: fully quantitative, semiquantitative, and qualitative assessment. JACC Cardiovasc Imaging. 2014; 7:14–22. PMID: 24433707.17. Greenwood JP, Motwani M, Maredia N, Brown JM, Everett CC, Nixon J, et al. Comparison of cardiovascular magnetic resonance and single-photon emission computed tomography in women with suspected coronary artery disease from the Clinical Evaluation of Magnetic Resonance imaging in Coronary heart disease (CE-MARC) trial. Circulation. 2014; 129:1129–1138. PMID: 24357404.
Article18. Motwani M, Maredia N, Fairbairn TA, Kozerke S, Greenwood JP, Plein S. Assessment of ischaemic burden in angiographic three-vessel coronary artery disease with high-resolution myocardial perfusion cardiovascular magnetic resonance imaging. Eur Heart J Cardiovasc Imaging. 2014; 15:701–708. PMID: 24493156.
Article19. Klem I, Heitner JF, Shah DJ, Sketch MH Jr, Behar V, Weinsaft J, et al. Improved detection of coronary artery disease by stress perfusion cardiovascular magnetic resonance with the use of delayed enhancement infarction imaging. J Am Coll Cardiol. 2006; 47:1630–1638. PMID: 16631001.
Article20. Li M, Zhou T, Yang LF, Peng ZH, Ding J, Sun G. Diagnostic accuracy of myocardial magnetic resonance perfusion to diagnose ischemic stenosis with fractional flow reserve as reference: systematic review and meta-analysis. JACC Cardiovasc Imaging. 2014; 7:1098–1105. PMID: 25306540.21. Pijls NH, Sels JW. Functional measurement of coronary stenosis. J Am Coll Cardiol. 2012; 59:1045–1057. PMID: 22421298.
Article22. Neglia D, Rovai D, Caselli C, Pietila M, Teresinska A, Aguadé-Bruix S, et al. EVINCI Study Investigators. Detection of significant coronary artery disease by noninvasive anatomical and functional imaging. Circ Cardiovasc Imaging. 2015; 8:pii: e002179.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of the Diagnostic Accuracies of 1.5T and 3T Stress Myocardial Perfusion Cardiovascular Magnetic Resonance for Detecting Significant Coronary Artery Disease
- Assessment of Myocardial Ischemia Using Stress Perfusion Cardiovascular Magnetic Resonance
- Stress Testing and Imaging Protocols for Myocardial Perfusion Studies
- Comparison of Stress-rest and Rest-stress One Day Myocardial Perfusion Scintigraphies in Detecting Coronary Artery Diseases
- Gender Difference of Accuracy in Detecting Coronary Artery Disease by Myocardial Perfusion SPECT