Single-Dose Gadoterate Meglumine for 3T Late Gadolinium Enhancement MRI for the Assessment of Chronic Myocardial Infarction: Intra-Individual Comparison with Conventional Double-Dose 1.5T MRI
- Affiliations
-
- 1Department of Radiology, Seoul National University Hospital, Seoul 03080, Korea. iameuna1@gmail.com
- KMID: 2410807
- DOI: http://doi.org/10.3348/kjr.2018.19.3.372
Abstract
OBJECTIVE
To intra-individually compare 3T magnetic resonance (MR) images obtained with one dose gadoterate meglumine to 1.5T MR using conventional double dose for assessment of chronic myocardial infarction.
MATERIALS AND METHODS
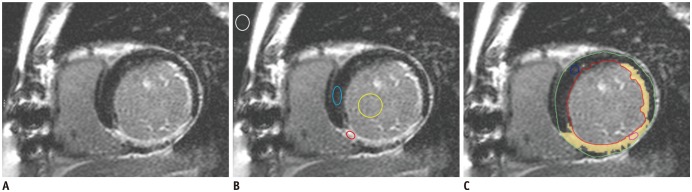
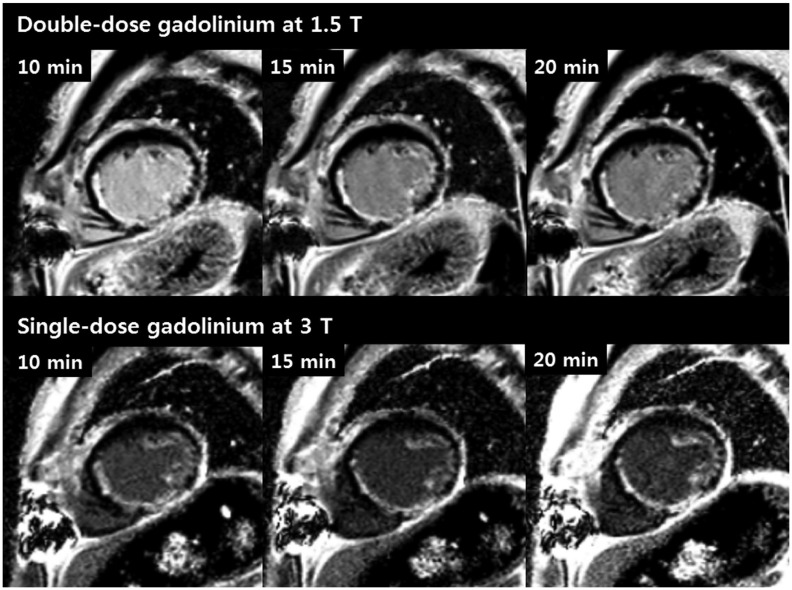
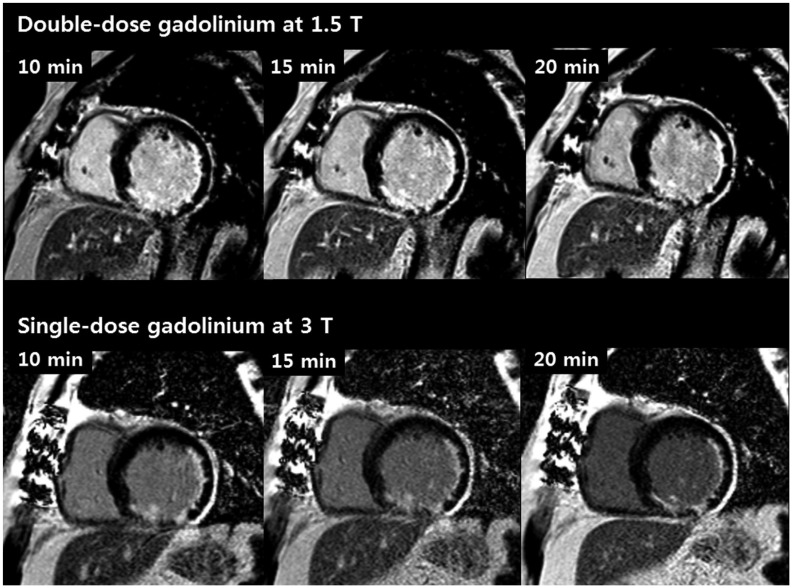
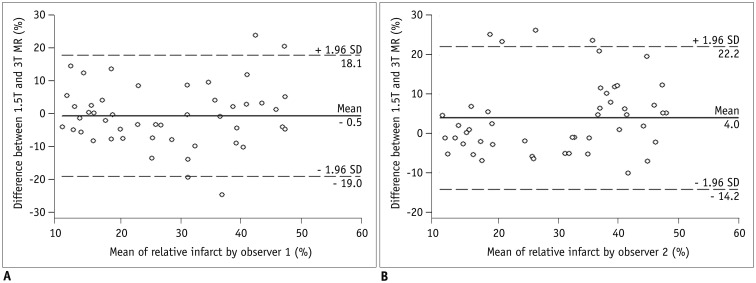
Sixteen patients diagnosed with chronic myocardial infarctions were examined on single-dose 3T MR within two weeks after undergoing double-dose 1.5T MR. Representative short-axis images were acquired at three points after administration of gadoterate meglumine. Contrast-to-noise ratios between infarcted and normal myocardium (CNRinfarct-normal) and between infarct and left ventricular cavity (CNRinfarct-LVC) were calculated and compared intra-individually at each temporal scan. Additionally, two independent readers assessed relative infarct size semi-automatically and inter-observer reproducibility was evaluated using intraclass correlation coefficient.
RESULTS
While higher CNRinfarct-normal was revealed at single-dose 3T at only 10 minutes scan (p = 0.047), the CNRinfarct-LVC was higher at single-dose 3T MR at each temporal scan (all, p < 0.05). Measurement of relative infarct size was not significantly different between both examinations for both observers (all, p > 0.05). However, inter-observer reproducibility was higher at single-dose 3T MR (all, p < 0.05).
CONCLUSION
Single-dose 3T MR is as effective as double-dose 1.5T MR for delineation of infarcted myocardium while being superior in detection of infarcted myocardium from the blood cavity, and provides better reproducibility for infarct size quantification.
Keyword
MeSH Terms
Figure
Cited by 4 articles
-
Guidelines for Cardiovascular Magnetic Resonance Imaging from the Korean Society of Cardiovascular Imaging—Part 2: Interpretation of Cine, Flow, and Angiography Data
Jae Wook Lee, Jee Hye Hur, Dong Hyun Yang, Bae Young Lee, Dong Jin Im, Su Jin Hong, Eun Young Kim, Eun-Ah Park, Yeseul Jo, JeongJae Kim, Chul Hwan Park, Hwan Seok Yong
Korean J Radiol. 2019;20(11):1477-1490. doi: 10.3348/kjr.2019.0407.Guideline for Cardiovascular Magnetic Resonance Imaging from the Korean Society of Cardiovascular Imaging—Part 1: Standardized Protocol
Yeseul Jo, JeongJae Kim, Chul Hwan Park, Jae Wook Lee, Jee Hye Hur, Dong Hyun Yang, Bae Young Lee, Dong Jin Im, Su Jin Hong, Eun Young Kim, Eun-Ah Park, Pan Ki Kim, Hwan Seok Yong
Korean J Radiol. 2019;20(9):1313-1333. doi: 10.3348/kjr.2019.0398.Guidelines for Cardiovascular Magnetic Resonance Imaging from the Korean Society of Cardiovascular Imaging—Part 3: Perfusion, Delayed Enhancement, and T1- and T2 Mapping
Dong Jin Im, Su Jin Hong, Eun-Ah Park, Eun Young Kim, Yeseul Jo, JeongJae Kim, Chul Hwan Park, Hwan Seok Yong, Jae Wook Lee, Jee Hye Hur, Dong Hyun Yang, Bae Young Lee
Korean J Radiol. 2019;20(12):1562-1582. doi: 10.3348/kjr.2019.0411.Guidelines for Cardiovascular Magnetic Resonance Imaging from the Korean Society of Cardiovascular Imaging (KOSCI) - Part 3: Perfusion, Delayed Enhancement, and T1- and T2 Mapping
Dong Jin Im, Su Jin Hong, Eun-Ah Park, Eun Young Kim, Yeseul Jo, Jeong Jae Kim, Chul Hwan Park, Hwan Seok Yong, Jae Wook Lee, Jee Hye Hur, Dong Hyun Yang, Bae-Young Lee
Investig Magn Reson Imaging. 2020;24(1):1-20. doi: 10.13104/imri.2020.24.1.1.
Reference
-
1. Kim RJ, Shah DJ, Judd RM. How we perform delayed enhancement imaging. J Cardiovasc Magn Reson. 2003; 5:505–514. PMID: 12882082.
Article2. Kim RJ, Wu E, Rafael A, Chen EL, Parker MA, Simonetti O, et al. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med. 2000; 343:1445–1453. PMID: 11078769.
Article3. Kim RJ, Fieno DS, Parrish TB, Harris K, Chen EL, Simonetti O, et al. Relationship of MRI delayed contrast enhancement to irreversible injury, infarct age, and contractile function. Circulation. 1999; 100:1992–2002. PMID: 10556226.
Article4. Nacif MS, Arai AE, Lima JA, Bluemke DA. Gadolinium-enhanced cardiovascular magnetic resonance: administered dose in relationship to United States Food and Drug Administration (FDA) guidelines. J Cardiovasc Magn Reson. 2012; 14:18. PMID: 22376193.
Article5. Cowper SE. Nephrogenic fibrosing dermopathy: the first 6 years. Curr Opin Rheumatol. 2003; 15:785–790. PMID: 14569211.
Article6. Thomsen HS, Marckmann P, Logager VB. Nephrogenic systemic fibrosis (NSF): a late adverse reaction to some of the gadolinium based contrast agents. Cancer Imaging. 2007; 7:130–137. PMID: 17905680.
Article7. Scheinfeld N. Nephrogenic fibrosing dermopathy: a comprehensive review for the dermatologist. Am J Clin Dermatol. 2006; 7:237–247. PMID: 16901184.8. Farrelly C, Rehwald W, Salerno M, Davarpanah A, Keeling AN, Jacobson JT, et al. Improved detection of subendocardial hyperenhancement in myocardial infarction using dark blood-pool delayed enhancement MRI. AJR Am J Roentgenol. 2011; 196:339–348. PMID: 21257885.
Article9. Wieben O, Francois C, Reeder SB. Cardiac MRI of ischemic heart disease at 3 T: potential and challenges. Eur J Radiol. 2008; 65:15–28. PMID: 18077119.
Article10. Klumpp B, Fenchel M, Hoevelborn T, Helber U, Scheule A, Claussen C, et al. Assessment of myocardial viability using delayed enhancement magnetic resonance imaging at 3.0 Tesla. Invest Radiol. 2006; 41:661–667. PMID: 16896300.
Article11. Haacke EM, Brown RW, Thompson MR, Venkatesan R. Magnetic resonance imaging: physical principles and sequence design. 1st ed. New Jersey: John Wiley & Sons;1999.12. Bottomley PA, Foster TH, Argersinger RE, Pfeifer LM. A review of normal tissue hydrogen NMR relaxation times and relaxation mechanisms from 1-100 MHz: dependence on tissue type, NMR frequency, temperature, species, excision, and age. Med Phys. 1984; 11:425–448. PMID: 6482839.
Article13. Cheng AS, Robson MD, Neubauer S, Selvanayagam JB. Irreversible myocardial injury: assessment with cardiovascular delayed-enhancement MR imaging and comparison of 1.5 and 3.0 T--initial experience. Radiology. 2007; 242:735–742. PMID: 17209167.
Article14. Flett AS, Hasleton J, Cook C, Hausenloy D, Quarta G, Ariti C, et al. Evaluation of techniques for the quantification of myocardial scar of differing etiology using cardiac magnetic resonance. JACC Cardiovasc Imaging. 2011; 4:150–156. PMID: 21329899.
Article15. De Cobelli F, Esposito A, Perseghin G, Sallemi C, Belloni E, Ravelli S, et al. Intraindividual comparison of gadobutrol and gadopentetate dimeglumine for detection of myocardial late enhancement in cardiac MRI. AJR Am J Roentgenol. 2012; 198:809–816. PMID: 22451545.
Article16. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174. PMID: 843571.
Article17. Kramer U, Fenchel M, Laub G, Seeger A, Klumpp B, Bretschneider C, et al. Low-dose, time-resolved, contrast-enhanced 3D MR angiography in the assessment of the abdominal aorta and its major branches at 3 Tesla. Acad Radiol. 2010; 17:564–576. PMID: 20171907.
Article18. Herborn CU, Runge VM, Watkins DM, Gendron JM, Naul LG. MR angiography of the renal arteries: intraindividual comparison of double-dose contrast enhancement at 1.5 T with standard dose at 3 T. AJR Am J Roentgenol. 2008; 190:173–177. PMID: 18094308.
Article19. Fratz S, Chung T, Greil GF, Samyn MM, Taylor AM, Valsangiacomo Buechel ER, et al. Guidelines and protocols for cardiovascular magnetic resonance in children and adults with congenital heart disease: SCMR expert consensus group on congenital heart disease. J Cardiovasc Magn Reson. 2013; 15:51. PMID: 23763839.
Article20. Kellman P, Arai AE, McVeigh ER, Aletras AH. Phase-sensitive inversion recovery for detecting myocardial infarction using gadolinium-delayed hyperenhancement. Magn Reson Med. 2002; 47:372–383. PMID: 11810682.
Article21. Idée JM, Port M, Raynal I, Schaefer M, Le Greneur S, Corot C. Clinical and biological consequences of transmetallation induced by contrast agents for magnetic resonance imaging: a review. Fundam Clin Pharmacol. 2006; 20:563–576. PMID: 17109649.
Article22. Ishiguchi T, Takahashi S. Safety of gadoterate meglumine (GdDOTA) as a contrast agent for magnetic resonance imaging: results of a post-marketing surveillance study in Japan. Drugs R D. 2010; 10:133–145. PMID: 20945944.23. Deray G, Rouviere O, Bacigalupo L, Maes B, Hannedouche T, Vrtovsnik F, et al. Safety of meglumine gadoterate (Gd-DOTA)-enhanced MRI compared to unenhanced MRI in patients with chronic kidney disease (RESCUE study). Eur Radiol. 2013; 23:1250–1259. PMID: 23212275.
Article24. Wagner M, Schilling R, Doeblin P, Huppertz A, Luhur R, Schwenke C, et al. Macrocyclic contrast agents for magnetic resonance imaging of chronic myocardial infarction: intraindividual comparison of gadobutrol and gadoterate meglumine. Eur Radiol. 2013; 23:108–114. PMID: 22772150.
Article25. Kim YK, Park EA, Lee W, Kim SY, Chung JW. Late gadolinium enhancement magnetic resonance imaging for the assessment of myocardial infarction: comparison of image quality between single and double doses of contrast agents. Int J Cardiovasc Imaging. 2014; 30(Suppl 2):129–135.
Article26. Kim HW, Rehwald WG, Wendell DC, Jenista E, Assche LV, Jensen CJ, et al. Flow-Independent Dark-blood DeLayed Enhancement (FIDDLE): validation of a novel black blood technique for the diagnosis of myocardial infarction. J Cardiovasc Magn Reson. 2016; 18(Suppl 1):055.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Single-Dose Gadoterate Meglumine for 3T Late Gadolinium Enhancement MRI for the Assessment of Chronic Myocardial Infarction: Intra-Individual Comparison with Conventional Double-Dose 1.5T MRI
- Contrast-enhanced Magnetic Resonance Imaging of Brain Metastases at 7.0T versus 1.5T: A Preliminary Result
- Usefulness of Contrast-Enhanced Magnetic Resonance Imaging in the Prediction of Myocardial Viability after Acute Myocardial Infarction
- Gd-DTPA Enhanced MRI of the Brain Infarction: Correlation between Onset of Infarction and Enhancing Patterns
- Diagnostic Accuracy and Evaluation of Myocardial Viability by Cardiac Magnetic Resonance Imaging in Acute Myocardial Infarction: A Comparison with Thallium-201 Myocardial SPECT