Ultrasonography-Based Thyroidal and Perithyroidal Anatomy and Its Clinical Significance
- Affiliations
-
- 1Department of Radiology, Ajou University School of Medicine, Suwon 443-380, Korea.
- 2Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul 138-736, Korea. radbaek@naver.com
- KMID: 2155548
- DOI: http://doi.org/10.3348/kjr.2015.16.4.749
Abstract
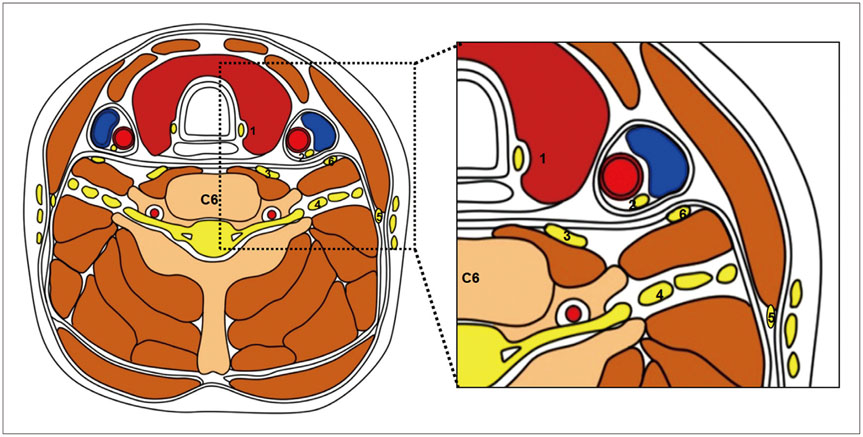
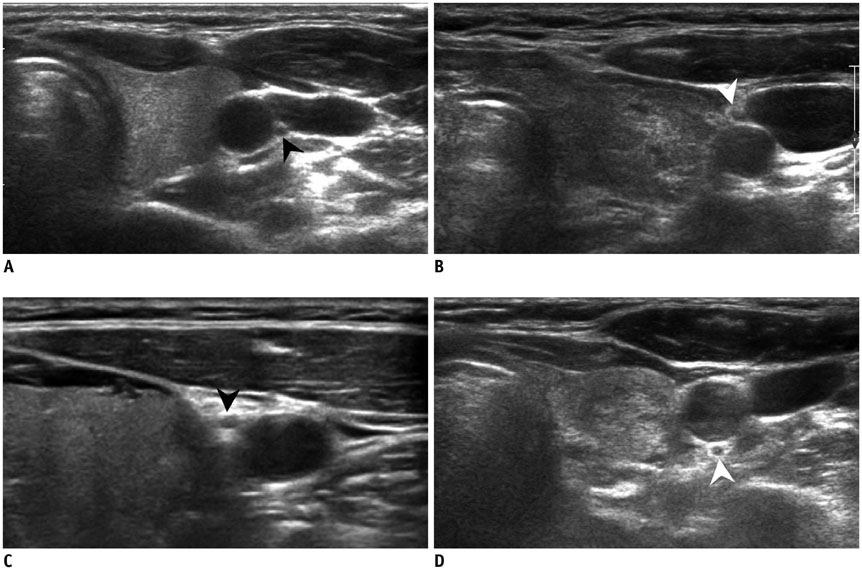
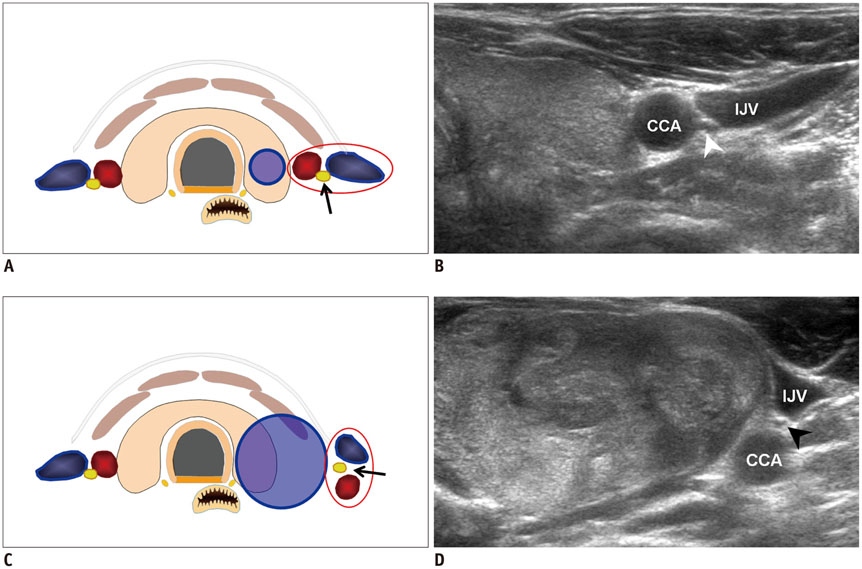
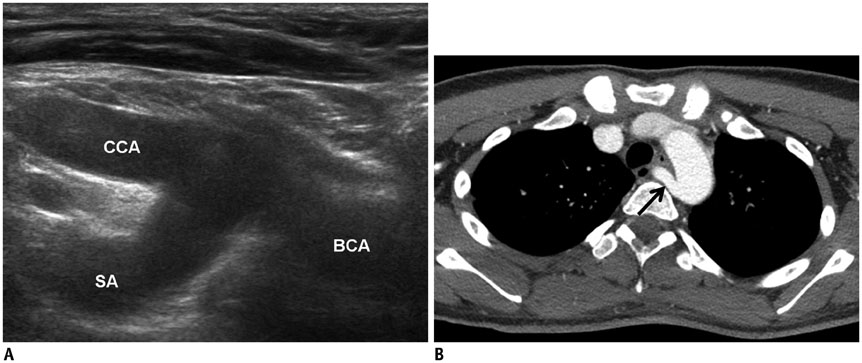
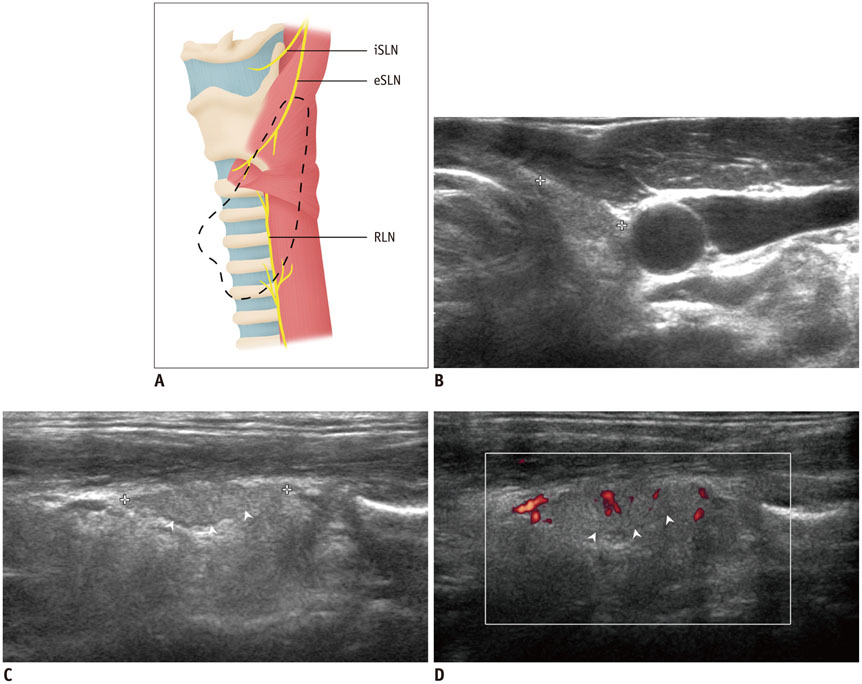
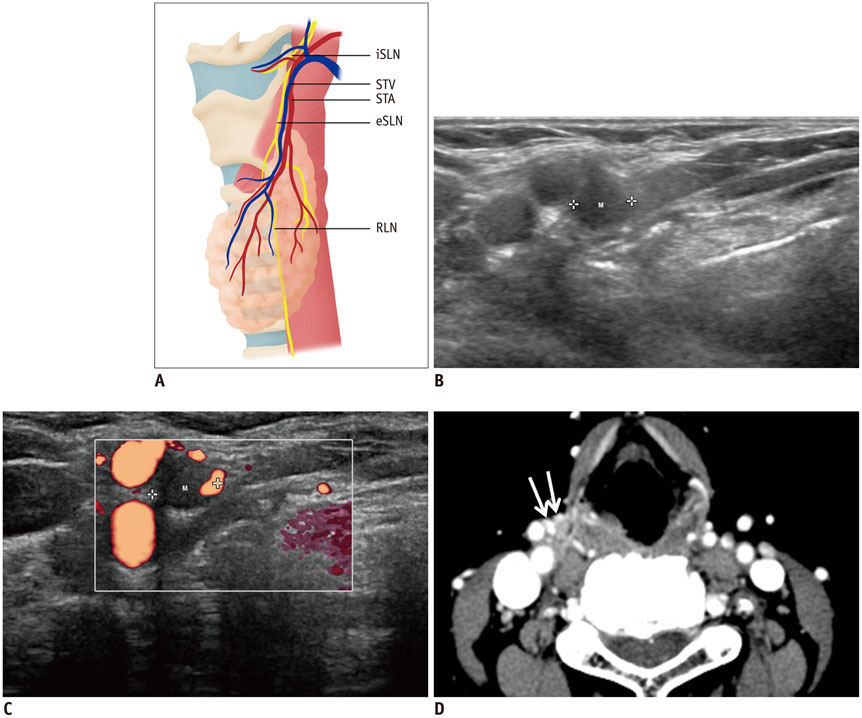
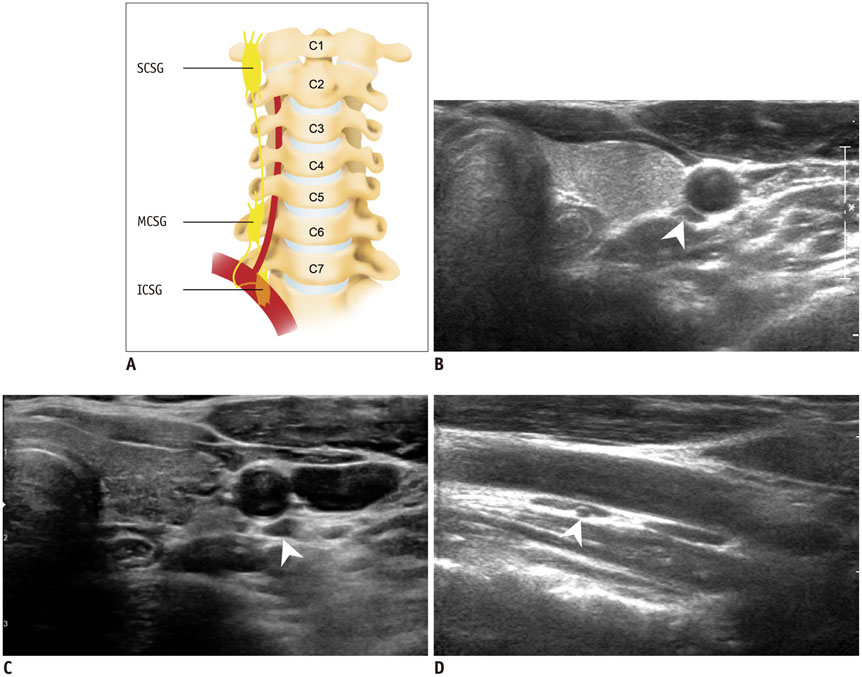
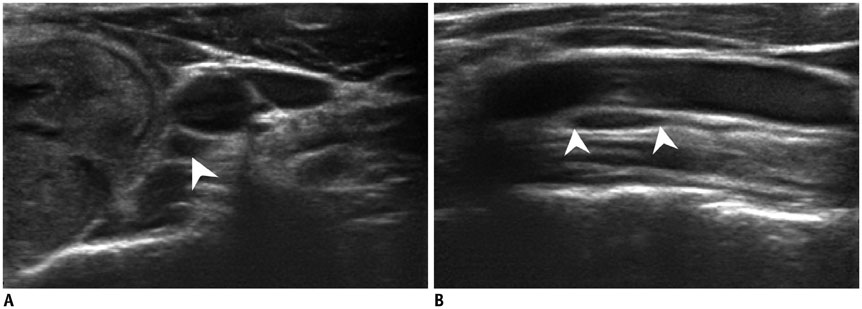
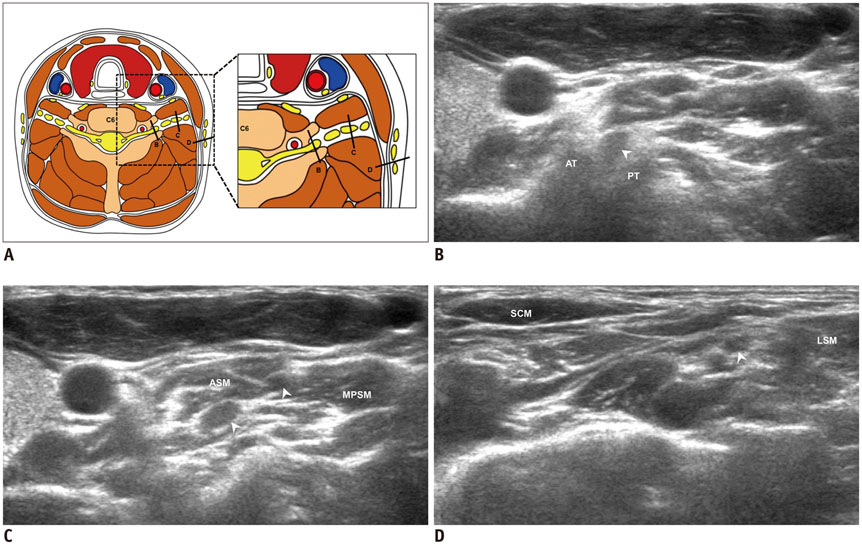
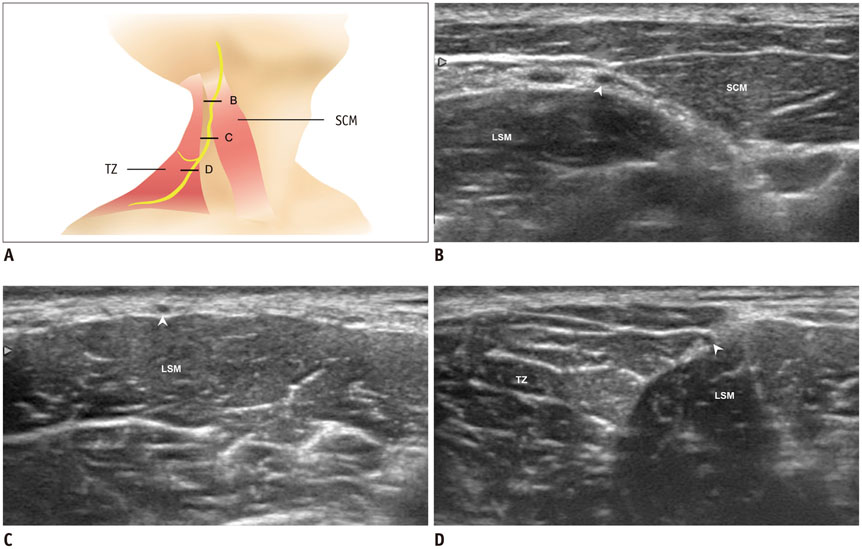
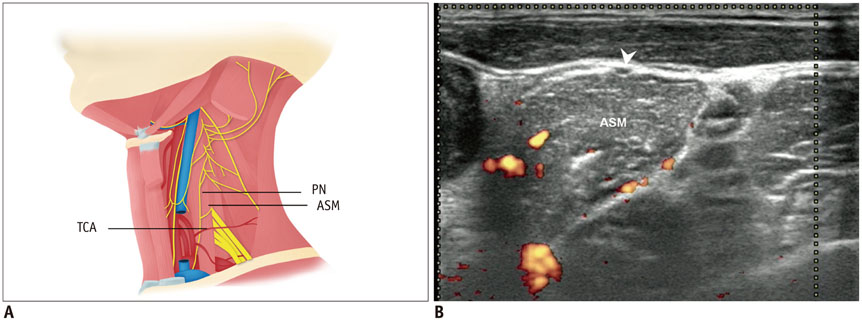
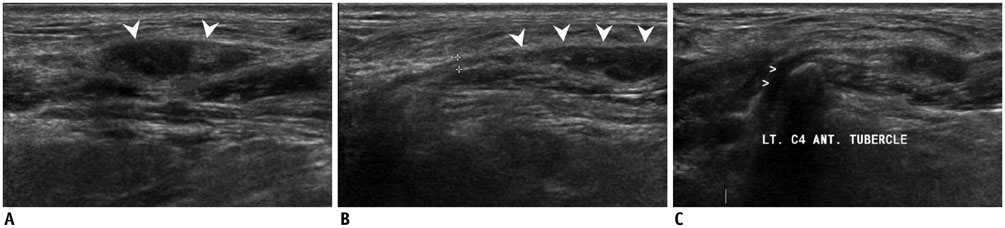
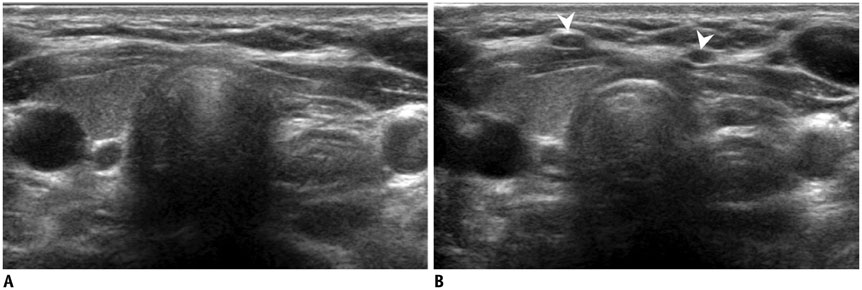
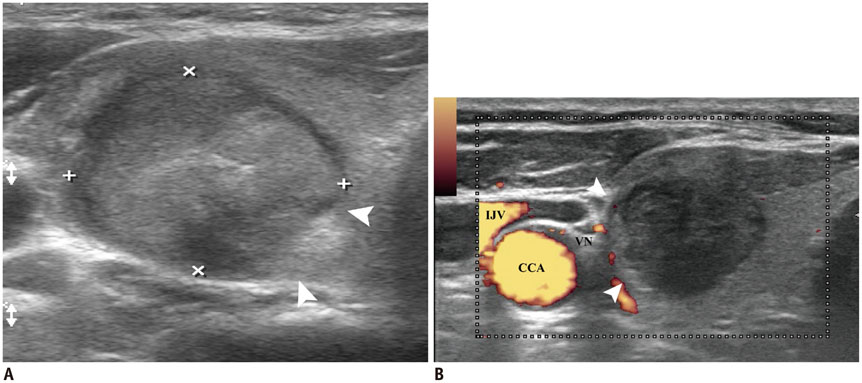
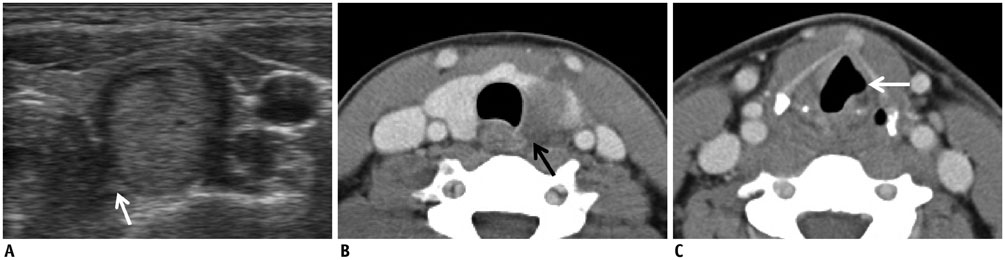
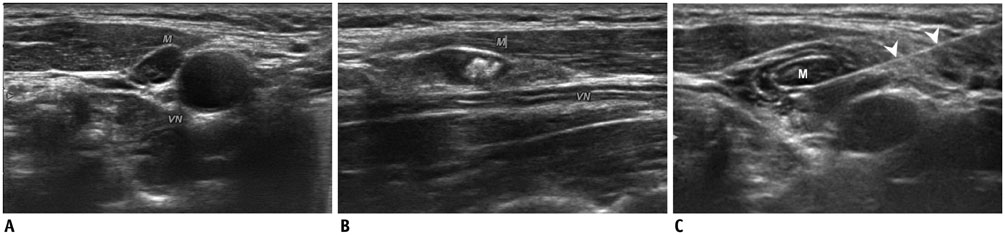
- Ultrasonography (US)-guided procedures such as ethanol ablation, radiofrequency ablation, laser ablation, selective nerve block, and core needle biopsy have been widely applied in the diagnosis and management of thyroid and neck lesions. For a safe and effective US-guided procedure, knowledge of neck anatomy, particularly that of the nerves, vessels, and other critical structures, is essential. However, most previous reports evaluated neck anatomy based on cadavers, computed tomography, or magnetic resonance imaging rather than US. Therefore, the aim of this article was to elucidate US-based thyroidal and perithyroidal anatomy, as well as its clinical significance in the use of prevention techniques for complications during the US-guided procedures. Knowledge of these areas may be helpful for maximizing the efficacy and minimizing the complications of US-guided procedures for the thyroid and other neck lesions.
Keyword
MeSH Terms
Figure
Cited by 9 articles
-
Effectiveness of Injecting Cold 5% Dextrose into Patients with Nerve Damage Symptoms during Thyroid Radiofrequency Ablation
Min Kyoung Lee, Jung Hwan Baek, Sae Rom Chung, Young Jun Choi, Yu-Mi Lee, Tae Yong Kim, Jeong Hyun Lee
Endocrinol Metab. 2020;35(2):407-415. doi: 10.3803/EnM.2020.35.2.407.A Comparison of Ultrasound-Guided Fine Needle Aspiration versus Core Needle Biopsy for Thyroid Nodules: Pain, Tolerability, and Complications
Eun Ji Jeong, Sae Rom Chung, Jung Hwan Baek, Young Jun Choi, Jae Kyun Kim, Jeong Hyun Lee
Endocrinol Metab. 2018;33(1):114-120. doi: 10.3803/EnM.2018.33.1.114.RE: 2017 Thyroid Radiofrequency Ablation Guideline: The Korean Society of Thyroid Radiology
Kai Lun Cheng, Wei-Che Lin
Korean J Radiol. 2018;19(6):1196-1197. doi: 10.3348/kjr.2018.19.6.1196.Recent Advances in Core Needle Biopsy for Thyroid Nodules
Chan Kwon Jung, Jung Hwan Baek
Endocrinol Metab. 2017;32(4):407-412. doi: 10.3803/EnM.2017.32.4.407.Revisiting Rupture of Benign Thyroid Nodules after Radiofrequency Ablation: Various Types and Imaging Features
Sae Rom Chung, Jung Hwan Baek, Jin Yong Sung, Ji Hwa Ryu, So Lyung Jung
Endocrinol Metab. 2019;34(4):415-421. doi: 10.3803/EnM.2019.34.4.415.Innovative Techniques for Image-Guided Ablation of Benign Thyroid Nodules: Combined Ethanol and Radiofrequency Ablation
Hye Sun Park, Jung Hwan Baek, Young Jun Choi, Jeong Hyun Lee
Korean J Radiol. 2017;18(3):461-469. doi: 10.3348/kjr.2017.18.3.461.Quality of Life in Patients Treated with Percutaneous Laser Ablation for Non-Functioning Benign Thyroid Nodules: A Prospective Single-Center Study
Silvia Oddo, Edineia Felix, Michele Mussap, Massimo Giusti
Korean J Radiol. 2018;19(1):175-184. doi: 10.3348/kjr.2018.19.1.175.2017 Thyroid Radiofrequency Ablation Guideline: Korean Society of Thyroid Radiology
Ji-hoon Kim, Jung Hwan Baek, Hyun Kyung Lim, Hye Shin Ahn, Seon Mi Baek, Yoon Jung Choi, Young Jun Choi, Sae Rom Chung, Eun Ju Ha, Soo Yeon Hahn, So Lyung Jung, Dae Sik Kim, Soo Jin Kim, Yeo Koon Kim, Chang Yoon Lee, Jeong Hyun Lee, Kwang Hwi Lee, Young Hen Lee, Jeong Seon Park, Hyesun Park, Jung Hee Shin, Chong Hyun Suh, Jin Yong Sung, Jung Suk Sim, Inyoung Youn, Miyoung Choi, Dong Gyu Na,
Korean J Radiol. 2018;19(4):632-655. doi: 10.3348/kjr.2018.19.4.632.2019 Practice guidelines for thyroid core needle biopsy: a report of the Clinical Practice Guidelines Development Committee of the Korean Thyroid Association
Chan Kwon Jung, Jung Hwan Baek, Dong Gyu Na, Young Lyun Oh, Ka Hee Yi, Ho-Cheol Kang
J Pathol Transl Med. 2020;54(1):64-86. doi: 10.4132/jptm.2019.12.04.
Reference
-
1. Gharib H, Hegedüs L, Pacella CM, Baek JH, Papini E. Clinical review: nonsurgical, image-guided, minimally invasive therapy for thyroid nodules. J Clin Endocrinol Metab. 2013; 98:3949–3957.2. Na DG, Lee JH, Jung SL, Kim JH, Sung JY, Shin JH, et al. Radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers: consensus statement and recommendations. Korean J Radiol. 2012; 13:117–125.3. Kapral S, Greher M, Huber G, Willschke H, Kettner S, Kdolsky R, et al. Ultrasonographic guidance improves the success rate of interscalene brachial plexus blockade. Reg Anesth Pain Med. 2008; 33:253–258.4. Soeding P, Eizenberg N. Review article: anatomical considerations for ultrasound guidance for regional anesthesia of the neck and upper limb. Can J Anaesth. 2009; 56:518–533.5. Yeon JS, Baek JH, Lim HK, Ha EJ, Kim JK, Song DE, et al. Thyroid nodules with initially nondiagnostic cytologic results: the role of core-needle biopsy. Radiology. 2013; 268:274–280.6. Na DG, Kim JH, Sung JY, Baek JH, Jung KC, Lee H, et al. Core-needle biopsy is more useful than repeat fine-needle aspiration in thyroid nodules read as nondiagnostic or atypia of undetermined significance by the Bethesda system for reporting thyroid cytopathology. Thyroid. 2012; 22:468–475.7. Lee SH, Kim MH, Bae JS, Lim DJ, Jung SL, Jung CK. Clinical outcomes in patients with non-diagnostic thyroid fine needle aspiration cytology: usefulness of the thyroid core needle biopsy. Ann Surg Oncol. 2014; 21:1870–1877.8. Trimboli P, Nasrollah N, Guidobaldi L, Taccogna S, Cicciarella Modica DD, Amendola S, et al. The use of core needle biopsy as first-line in diagnosis of thyroid nodules reduces false negative and inconclusive data reported by fine-needle aspiration. World J Surg Oncol. 2014; 12:61.9. Ha EJ, Baek JH, Lee JH, Kim JK, Kim JK, Lim HK, et al. Core needle biopsy can minimise the non-diagnostic results and need for diagnostic surgery in patients with calcified thyroid nodules. Eur Radiol. 2014; 24:1403–1409.10. Ha EJ, Baek JH, Lee JH, Song DE, Kim JK, Shong YK, et al. Sonographically suspicious thyroid nodules with initially benign cytologic results: the role of a core needle biopsy. Thyroid. 2013; 23:703–708.11. Kim BM, Kim EK, Kim MJ, Yang WI, Park CS, Park SI. Sonographically guided core needle biopsy of cervical lymphadenopathy in patients without known malignancy. J Ultrasound Med. 2007; 26:585–591.12. Screaton NJ, Berman LH, Grant JW. Head and neck lymphadenopathy: evaluation with US-guided cutting-needle biopsy. Radiology. 2002; 224:75–81.13. Baek JH, Lee JH, Sung JY, Bae JI, Kim KT, Sim J, et al. Complications encountered in the treatment of benign thyroid nodules with US-guided radiofrequency ablation: a multicenter study. Radiology. 2012; 262:335–342.14. Kaufman MR, Elkwood AI, Rose MI, Patel T, Ashinoff R, Fields R, et al. Surgical treatment of permanent diaphragm paralysis after interscalene nerve block for shoulder surgery. Anesthesiology. 2013; 119:484–487.15. Jeng CL, Torrillo TM, Rosenblatt MA. Complications of peripheral nerve blocks. Br J Anaesth. 2010; 105:Suppl 1. i97–i107.16. Usui Y, Kobayashi T, Kakinuma H, Watanabe K, Kitajima T, Matsuno K. An anatomical basis for blocking of the deep cervical plexus and cervical sympathetic tract using an ultrasound-guided technique. Anesth Analg. 2010; 110:964–968.17. Bhatia A, Flamer D, Peng PW. Evaluation of sonoanatomy relevant to performing stellate ganglion blocks using anterior and lateral simulated approaches: an observational study. Can J Anaesth. 2012; 59:1040–1047.18. Chiou HJ, Chou YH, Chiou SY, Liu JB, Chang CY. Peripheral nerve lesions: role of high-resolution US. Radiographics. 2003; 23:e15.19. Fornage BD. Peripheral nerves of the extremities: imaging with US. Radiology. 1988; 167:179–182.20. Giovagnorio F, Martinoli C. Sonography of the cervical vagus nerve: normal appearance and abnormal findings. AJR Am J Roentgenol. 2001; 176:745–749.21. Knappertz VA, Tegeler CH, Hardin SJ, McKinney WM. Vagus nerve imaging with ultrasound: anatomic and in vivo validation. Otolaryngol Head Neck Surg. 1998; 118:82–85.22. Donatini G, Iacconi P, De Bartolomeis C, Iacconi C, Fattori S, Pucci A, et al. Neck lesions mimicking thyroid pathology. Langenbecks Arch Surg. 2009; 394:435–440.23. Ha EJ, Baek JH, Lee JH, Kim JK, Shong YK. Clinical significance of vagus nerve variation in radiofrequency ablation of thyroid nodules. Eur Radiol. 2011; 21:2151–2157.24. Ha EJ, Baek JH, Lee JH, Kim YJ, Kim JK, Kim TY, et al. Characteristic ultrasound feature of traumatic neuromas after neck dissection: direct continuity with the cervical plexus. Thyroid. 2012; 22:820–826.25. Park JK, Jeong SY, Lee JH, Lim GC, Chang JW. Variations in the course of the cervical vagus nerve on thyroid ultrasonography. AJNR Am J Neuroradiol. 2011; 32:1178–1181.26. Le Corroller T, Sebag F, Vidal V, Jacquier A, Champsaur P, Bartoli JM, et al. Sonographic diagnosis of a cervical vagal schwannoma. J Clin Ultrasound. 2009; 37:57–60.27. Mra Z, Wax MK. Nonrecurrent laryngeal nerves: anatomic considerations during thyroid and parathyroid surgery. Am J Otolaryngol. 1999; 20:91–95.28. Henry JF, Audiffret J, Denizot A, Plan M. The nonrecurrent inferior laryngeal nerve: review of 33 cases, including two on the left side. Surgery. 1988; 104:977–984.29. Gray SW, Skandalakis JE, Akin JT Jr. Embryological considerations of thyroid surgery: developmental anatomy of the thyroid, parathyroids and the recurrent laryngeal nerve. Am Surg. 1976; 42:621–628.30. Avisse C, Marcus C, Delattre JF, Marcus C, Cailliez-Tomasi JP, Palot JP, et al. Right nonrecurrent inferior laryngeal nerve and arteria lusoria: the diagnostic and therapeutic implications of an anatomic anomaly. Review of 17 cases. Surg Radiol Anat. 1998; 20:227–232.31. Gong RX, Luo SH, Gong YP, Wei T, Li ZH, Huang JB, et al. Prediction of nonrecurrent laryngeal nerve before thyroid surgery--experience with 1825 cases. J Surg Res. 2014; 189:75–80.32. Yetisir F, Salman AE, Çiftçi B, Teber A, Kiliç M. Efficacy of ultrasonography in identification of non-recurrent laryngeal nerve. Int J Surg. 2012; 10:506–509.33. Huang SM, Wu TJ. Neck ultrasound for prediction of right nonrecurrent laryngeal nerve. Head Neck. 2010; 32:844–849.34. Tomoda C, Takamura Y, Ito Y, Miya A, Miyauchi A. Transient vocal cord paralysis after fine-needle aspiration biopsy of thyroid tumor. Thyroid. 2006; 16:697–699.35. Shin JE, Baek JH, Lee JH. Radiofrequency and ethanol ablation for the treatment of recurrent thyroid cancers: current status and challenges. Curr Opin Oncol. 2013; 25:14–19.36. Shin JH, Baek JH, Ha EJ, Lee JH. Radiofrequency ablation of thyroid nodules: basic principles and clinical application. Int J Endocrinol. 2012; 2012:919650.37. Sasou S, Nakamura S, Kurihara H. Suspensory ligament of Berry: its relationship to recurrent laryngeal nerve and anatomic examination of 24 autopsies. Head Neck. 1998; 20:695–698.38. Barberet G, Henry Y, Tatu L, Berthier F, Besch G, Pili-Floury S, et al. Ultrasound description of a superior laryngeal nerve space as an anatomical basis for echoguided regional anaesthesia. Br J Anaesth. 2012; 109:126–128.39. Saylam CY, Ozgiray E, Orhan M, Cagli S, Zileli M. Neuroanatomy of cervical sympathetic trunk: a cadaveric study. Clin Anat. 2009; 22:324–330.40. Shin JE, Baek JH, Ha EJ, Choi YJ, Choi WJ, Lee JH. Ultrasound features of middle cervical sympathetic ganglion. Clin J Pain. 2014; 11. 19. [Epub ahead of print].41. Kiray A, Arman C, Naderi S, Güvencer M, Korman E. Surgical anatomy of the cervical sympathetic trunk. Clin Anat. 2005; 18:179–185.42. Gofeld M, Bhatia A, Abbas S, Ganapathy S, Johnson M. Development and validation of a new technique for ultrasound-guided stellate ganglion block. Reg Anesth Pain Med. 2009; 34:475–479.43. Pishdad GR, Pishdad P, Pishdad R. Horner's syndrome as a complication of percutaneous ethanol treatment of thyroid nodule. Thyroid. 2011; 21:327–328.44. Messika O, Telman G. Horner syndrome after lymph node fine needle aspiration. Acta Cytol. 2009; 53:487–488.45. Lee JH, Lee HK, Lee DH, Choi CG, Kim SJ, Suh DC. Neuroimaging strategies for three types of Horner syndrome with emphasis on anatomic location. AJR Am J Roentgenol. 2007; 188:W74–W81.46. Gervasio A, Mujahed I, Biasio A, Alessi S. Ultrasound anatomy of the neck: the infrahyoid region. J Ultrasound. 2010; 13:85–89.47. Ihnatsenka B, Boezaart AP. Applied sonoanatomy of the posterior triangle of the neck. Int J Shoulder Surg. 2010; 4:63–74.48. Roessel T, Wiessner D, Heller AR, Zimmermann T, Koch T, Litz RJ. High-resolution ultrasound-guided high interscalene plexus block for carotid endarterectomy. Reg Anesth Pain Med. 2007; 32:247–253.49. Narouze S. Sonoanatomy of the cervical spinal nerve roots: implications for brachial plexus block. Reg Anesth Pain Med. 2009; 34:616.50. Demondion X, Herbinet P, Boutry N, Fontaine C, Francke JP, Cotten A. Sonographic mapping of the normal brachial plexus. AJNR Am J Neuroradiol. 2003; 24:1303–1309.51. Canella C, Demondion X, Abreu E, Marchiori E, Cotten H, Cotten A. Anatomical study of spinal accessory nerve using ultrasonography. Eur J Radiol. 2013; 82:56–61.52. Mirjalili SA, Muirhead JC, Stringer MD. Ultrasound visualization of the spinal accessory nerve in vivo. J Surg Res. 2012; 175:e11–e16.53. Seok JI, Kim JW, Walker FO. Spontaneous spinal accessory nerve palsy: the diagnostic usefulness of ultrasound. Muscle Nerve. 2014; 50:149–150.54. Hong MJ, Baek JH, Kim DY, Ha EJ, Choi WJ, Choi YJ, et al. Spinal accessory nerve: ultrasound findings and correlations with neck lymph node levels. Ultraschall Med. 2014; 12. 17. [Epub ahead of print].55. Canella C, Demondion X, Delebarre A, Moraux A, Cotten H, Cotten A. Anatomical study of phrenic nerve using ultrasound. Eur Radiol. 2010; 20:659–665.56. Kuusniemi K, Pyylampi V. Phrenic nerve block with ultrasound-guidance for treatment of hiccups: a case report. J Med Case Rep. 2011; 5:493.57. Kang KN, Park IK, Suh JH, Leem JG, Shin JW. Ultrasound-guided Pulsed Radiofrequency Lesioning of the Phrenic Nerve in a Patient with Intractable Hiccup. Korean J Pain. 2010; 23:198–201.58. Ha EJ, Lee JH, Lim HK, Bae Kim W, Baek JH. Identification of continuity of transected nerve on sonography after neck dissection: direct sign of traumatic neuroma. Thyroid. 2011; 21:1385–1387.59. Standring S. Gray's Anatomy: The Anatomical Basis of Clinical Practice, Expert Consult. London: Churchill Livingstone;2008.60. Jacob S. Human anatomy: A Clinically-Orientated Approach. New York: Elsevier;2008.61. Singh M, Chin KJ, Chan VW, Wong DT, Prasad GA, Yu E. Use of sonography for airway assessment: an observational study. J Ultrasound Med. 2010; 29:79–85.62. van Eerd M, Patijn J, Sieben JM, Sommer M, Van Zundert J, van Kleef M, et al. Ultrasonography of the cervical spine: an in vitro anatomical validation model. Anesthesiology. 2014; 120:86–96.63. Strauss S. Cricoid cartilage masquerading as a tumour on thyroid ultrasound. Br J Radiol. 1999; 72:644–647.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasonography-Based Thyroidal and Perithyroidal Anatomy and Its Clinical Significance
- Real-Time US Diagnosis for Perithyroidal Invasion of Thyroid Malignancy
- The Clinical Significance of a Minimal Extra-thyroidal Extension of Papillary Thyroid Cancer for the Recurrence of Regional Cervical Lymph Nodes
- Incidentally diagnosed Takayasu arteritis on thyroid ultrasonography showing prominent collateral vessels of thyroidal arteries and common carotid artery occlusion
- Ultrasonography of the lower extremity veins: anatomy and basic approach