Korean J Radiol.
2014 Dec;15(6):836-843. 10.3348/kjr.2014.15.6.836.
Moving-Shot versus Fixed Electrode Techniques for Radiofrequency Ablation: Comparison in an Ex-Vivo Bovine Liver Tissue Model
- Affiliations
-
- 1Department of Radiology and the Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul 138-736, Korea. radbaek@naver.com
- 2Department of Radiology, Ajou University School of Medicine, Suwon 443-380, Korea.
- KMID: 1794657
- DOI: http://doi.org/10.3348/kjr.2014.15.6.836
Abstract
OBJECTIVE
To compare the ablation characteristics of the moving-shot technique (MST) and the fixed electrode technique (FET) for radiofrequency (RF) ablation in an ex-vivo bovine liver tissue model.
MATERIALS AND METHODS
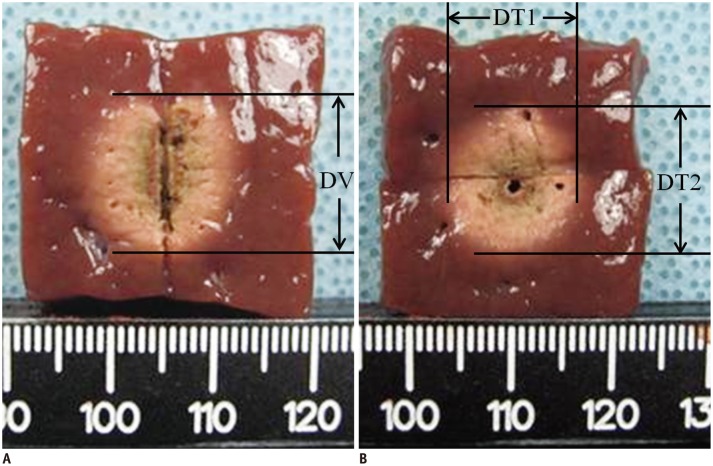
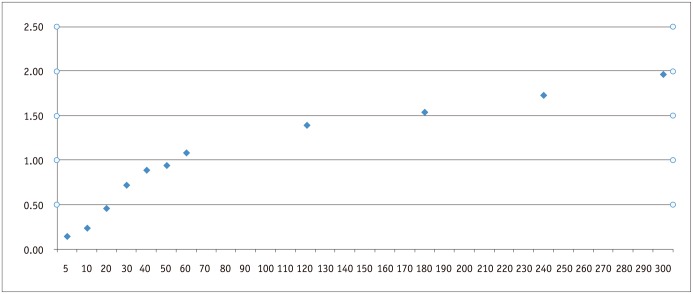
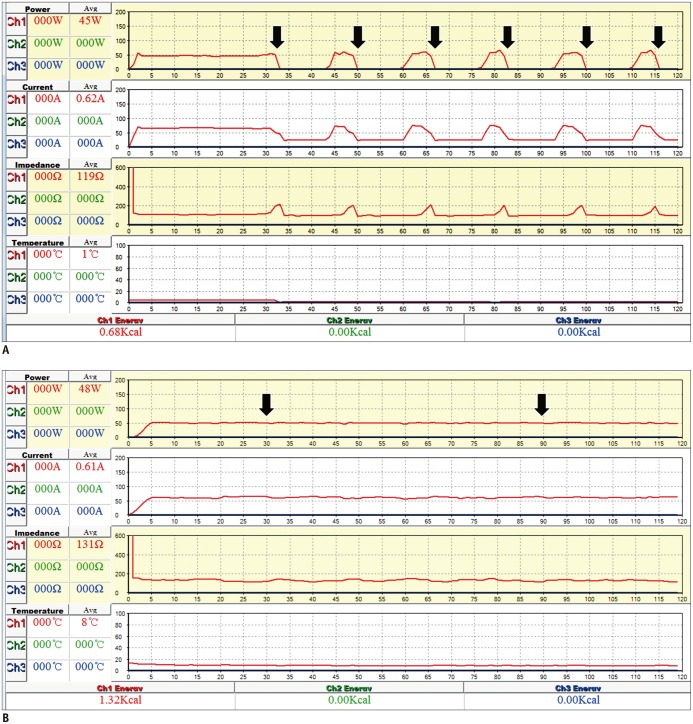
We performed RF ablation using FET in 110 bovine liver blocks using 11 different ablation times ranging from 5 seconds to 5 minutes (10 blocks per each time duration). Ten bovine liver blocks at each ablation time of 1- or 2-minute, were ablated with MST, which treated conceptual ablation units by moving the electrode tip. We evaluated the ablation volume obtained with FET across ablation time lengths. The results of FET and MST performed with the same ablation time lengths, i.e., 1- and 2-minute ablation time were also compared.
RESULTS
The ablation volume achieved with FET gradually increased with increasing ablation time; however, the pair-wise statistical comparison between 2 neighboring ablation time lengths was not significant after 30 seconds. MST with either 1- or 2-minute ablation time achieved larger ablation volumes (1.1 +/- 0.2 mL vs. 2.7 +/- 0.3 mL, p < 0.001; and 1.4 +/- 0.2 mL vs. 5.6 +/- 0.4 mL, p < 0.001, respectively), longer true RF times (46.7 +/- 4.6 seconds vs. 60 seconds, p < 0.001; and 64.8 +/- 4.6 seconds vs. 120 seconds, p < 0.001, respectively), fewer numbers of RF cut-offs (1.6 +/- 0.5 vs. 0, p < 0.001; and 5.5 +/- 0.5 vs. 0, p < 0.001, respectively), and greater energy deposition (2050.16 +/- 209.2 J vs. 2677.76 +/- 83.68 J, p < 0.001; and 2970.64 +/- 376.56 J vs. 5564.72 +/- 5439.2 J, p < 0.001, respectively), than FET.
CONCLUSION
The MST can achieve a larger ablation volume by preventing RF cut-off, compared with the FET in an ex-vivo bovine liver model.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Ultrasound (US)-Guided Ablation of Thyroid Nodules
Byung Seup Kim
J Surg Ultrasound. 2023;10(1):14-23. doi: 10.46268/jsu.2023.10.1.14.
Reference
-
1. Dupuy DE, Zagoria RJ, Akerley W, Mayo-Smith WW, Kavanagh PV, Safran H. Percutaneous radiofrequency ablation of malignancies in the lung. AJR Am J Roentgenol. 2000; 174:57–59. PMID: 10628454.
Article2. Dupuy DE, Goldberg SN. Image-guided radiofrequency tumor ablation: challenges and opportunities--part II. J Vasc Interv Radiol. 2001; 12:1135–1148. PMID: 11585879.
Article3. Gazelle GS, Goldberg SN, Solbiati L, Livraghi T. Tumor ablation with radio-frequency energy. Radiology. 2000; 217:633–646. PMID: 11110923.
Article4. Kang TW, Rhim H, Kim EY, Kim YS, Choi D, Lee WJ, et al. Percutaneous radiofrequency ablation for the hepatocellular carcinoma abutting the diaphragm: assessment of safety and therapeutic efficacy. Korean J Radiol. 2009; 10:34–42. PMID: 19182501.
Article5. Goldberg SN. Radiofrequency tumor ablation: principles and techniques. Eur J Ultrasound. 2001; 13:129–147. PMID: 11369525.
Article6. Goldberg SN, Gazelle GS, Mueller PR. Thermal ablation therapy for focal malignancy: a unified approach to underlying principles, techniques, and diagnostic imaging guidance. AJR Am J Roentgenol. 2000; 174:323–331. PMID: 10658699.7. Rhim H, Goldberg SN, Dodd GD 3rd, Solbiati L, Lim HK, Tonolini M, et al. Essential techniques for successful radio-frequency thermal ablation of malignant hepatic tumors. Radiographics. 2001; 21 Spec No:S17–S35. PMID: 11598245.
Article8. Baek JH, Kim YS, Lee D, Huh JY, Lee JH. Benign predominantly solid thyroid nodules: prospective study of efficacy of sonographically guided radiofrequency ablation versus control condition. AJR Am J Roentgenol. 2010; 194:1137–1142. PMID: 20308523.
Article9. Baek JH, Kim YS, Sung JY, Choi H, Lee JH. Locoregional control of metastatic well-differentiated thyroid cancer by ultrasound-guided radiofrequency ablation. AJR Am J Roentgenol. 2011; 197:W331–W336. PMID: 21785061.
Article10. Baek JH, Moon WJ, Kim YS, Lee JH, Lee D. Radiofrequency ablation for the treatment of autonomously functioning thyroid nodules. World J Surg. 2009; 33:1971–1977. PMID: 19575141.
Article11. Jeong WK, Baek JH, Rhim H, Kim YS, Kwak MS, Jeong HJ, et al. Radiofrequency ablation of benign thyroid nodules: safety and imaging follow-up in 236 patients. Eur Radiol. 2008; 18:1244–1250. PMID: 18286289.
Article12. Lee JH, Kim YS, Lee D, Choi H, Yoo H, Baek JH. Radiofrequency ablation (RFA) of benign thyroid nodules in patients with incompletely resolved clinical problems after ethanol ablation (EA). World J Surg. 2010; 34:1488–1493. PMID: 20376445.
Article13. Sung JY, Kim YS, Choi H, Lee JH, Baek JH. Optimum first-line treatment technique for benign cystic thyroid nodules: ethanol ablation or radiofrequency ablation? AJR Am J Roentgenol. 2011; 196:W210–W214. PMID: 21257865.
Article14. Baek JH, Lee JH, Valcavi R, Pacella CM, Rhim H, Na DG. Thermal ablation for benign thyroid nodules: radiofrequency and laser. Korean J Radiol. 2011; 12:525–540. PMID: 21927553.
Article15. Ha EJ, Baek JH, Lee JH. The efficacy and complications of radiofrequency ablation of thyroid nodules. Curr Opin Endocrinol Diabetes Obes. 2011; 18:310–314. PMID: 21841482.
Article16. Baek JH, Jeong HJ, Kim YS, Kwak MS, Lee D. Radiofrequency ablation for an autonomously functioning thyroid nodule. Thyroid. 2008; 18:675–676. PMID: 18578625.
Article17. Baek JH, Lee JH, Sung JY, Bae JI, Kim KT, Sim J, et al. Complications encountered in the treatment of benign thyroid nodules with US-guided radiofrequency ablation: a multicenter study. Radiology. 2012; 262:335–342. PMID: 21998044.
Article18. Spiezia S, Garberoglio R, Milone F, Ramundo V, Caiazzo C, Assanti AP, et al. Thyroid nodules and related symptoms are stably controlled two years after radiofrequency thermal ablation. Thyroid. 2009; 19:219–225. PMID: 19265492.
Article19. Ha EJ, Baek JH, Lee JH, Kim JK, Shong YK. Clinical significance of vagus nerve variation in radiofrequency ablation of thyroid nodules. Eur Radiol. 2011; 21:2151–2157. PMID: 21633824.
Article20. Na DG, Lee JH, Jung SL, Kim JH, Sung JY, Shin JH, et al. Radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers: consensus statement and recommendations. Korean J Radiol. 2012; 13:117–125. PMID: 22438678.
Article21. Lee JD, Lee JM, Kim SW, Kim CS, Mun WS. MR imaging-histopathologic correlation of radiofrequency thermal ablation lesion in a rabbit liver model: observation during acute and chronic stages. Korean J Radiol. 2001; 2:151–158. PMID: 11752986.
Article22. Morimoto M, Sugimori K, Shirato K, Kokawa A, Tomita N, Saito T, et al. Treatment of hepatocellular carcinoma with radiofrequency ablation: radiologic-histologic correlation during follow-up periods. Hepatology. 2002; 35:1467–1475. PMID: 12029632.
Article23. Clasen S, Schmidt D, Dietz K, Boss A, Kröber SM, Schraml C, et al. Bipolar radiofrequency ablation using internally cooled electrodes in ex vivo bovine liver: prediction of coagulation volume from applied energy. Invest Radiol. 2007; 42:29–36. PMID: 17213746.24. Crocetti L, Lencioni R, Debeni S, See TC, Pina CD, Bartolozzi C. Targeting liver lesions for radiofrequency ablation: an experimental feasibility study using a CT-US fusion imaging system. Invest Radiol. 2008; 43:33–39. PMID: 18097275.25. Lee JM, Han JK, Kim HC, Choi YH, Kim SH, Choi JY, et al. Switching monopolar radiofrequency ablation technique using multiple, internally cooled electrodes and a multichannel generator: ex vivo and in vivo pilot study. Invest Radiol. 2007; 42:163–171. PMID: 17287646.26. Lee JM, Han JK, Kim HC, Kim SH, Kim KW, Joo SM, et al. Multiple-electrode radiofrequency ablation of in vivo porcine liver: comparative studies of consecutive monopolar, switching monopolar versus multipolar modes. Invest Radiol. 2007; 42:676–683. PMID: 17984764.27. Lee JM, Han JK, Kim SH, Shin KS, Lee JY, Park HS, et al. Comparison of wet radiofrequency ablation with dry radiofrequency ablation and radiofrequency ablation using hypertonic saline preinjection: ex vivo bovine liver. Korean J Radiol. 2004; 5:258–265. PMID: 15637476.
Article28. Na DG, Lee JH, Kim SM, Lim HK, Baek JH. Unidirectional ablation electrode to minimize thermal injury during radiofrequency ablation: an experimental study in an ex vivo bovine liver model. J Vasc Interv Radiol. 2011; 22:935–940. PMID: 21530310.
Article29. Haemmerich D, Laeseke PF. Thermal tumour ablation: devices, clinical applications and future directions. Int J Hyperthermia. 2005; 21:755–760. PMID: 16338858.
Article30. Jang SW, Baek JH, Kim JK, Sung JY, Choi H, Lim HK, et al. How to manage the patients with unsatisfactory results after ethanol ablation for thyroid nodules: role of radiofrequency ablation. Eur J Radiol. 2012; 81:905–910. PMID: 21388767.
Article31. Huh JY, Baek JH, Choi H, Kim JK, Lee JH. Symptomatic benign thyroid nodules: efficacy of additional radiofrequency ablation treatment session--prospective randomized study. Radiology. 2012; 263:909–916. PMID: 22438360.
Article32. Gharib H, Hegedüs L, Pacella CM, Baek JH, Papini E. Clinical review: nonsurgical, image-guided, minimally invasive therapy for thyroid nodules. J Clin Endocrinol Metab. 2013; 98:3949–3957. PMID: 23956350.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Moving-Shot versus Fixed Electrode Techniques for Radiofrequency Ablation: Comparison in an Ex-Vivo Bovine Liver Tissue Model
- Overlapping Ablation Using a Coaxial Radiofrequency Electrode and Multiple Cannulae System: Experimental Study in ex-Vivo Bovine Liver
- Radiofrequency Tissue Ablation with Cooled-Tip Electrodes:An Experimental Study in a Bovine Liver Model on Variables Influencing Lesion Size
- Novel and Advanced Ultrasound Techniques for Thyroid Thermal Ablation
- Radiofrequency Thermal Ablation of Hepatocellular Carcinomas