J Korean Med Sci.
2013 Jan;28(1):42-47. 10.3346/jkms.2013.28.1.42.
Pediatric Liver Transplantation Outcomes in Korea
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. sklee3464@skku.edu
- 2Department of Pediatrics, Asan Medical Center Children's Hospital, University of Ulsan College of Medicine, Seoul, Korea.
- 3Department of Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 4Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 5Department of Surgery, Yonsei University College of Medicine, Seoul, Korea.
- 6Department of Surgery, Division of Hepatobiliary Surgery and Liver Transplantation, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2157999
- DOI: http://doi.org/10.3346/jkms.2013.28.1.42
Abstract
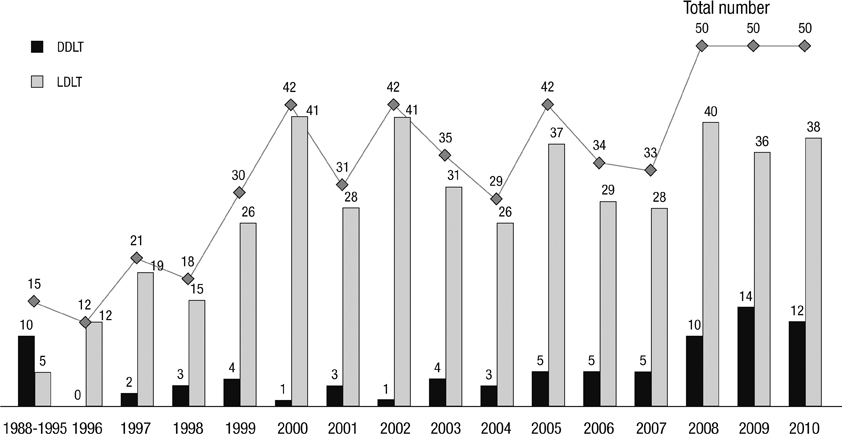
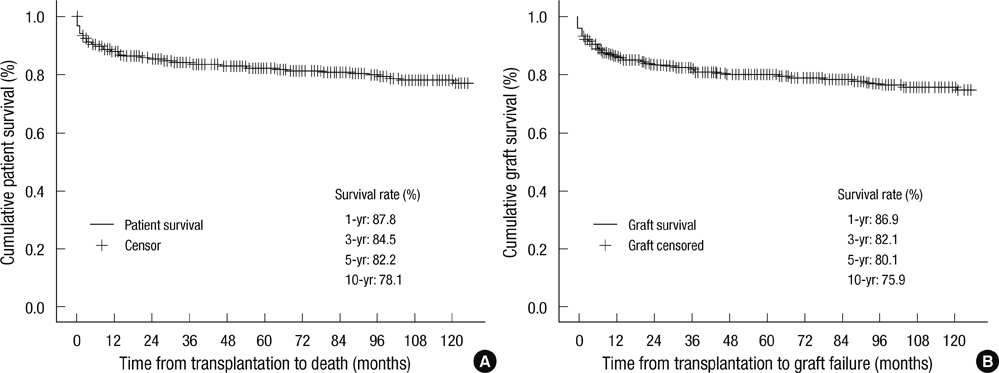
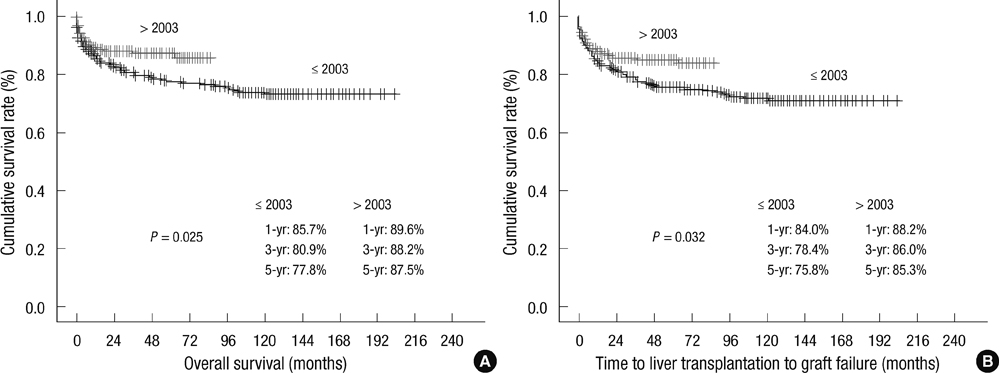
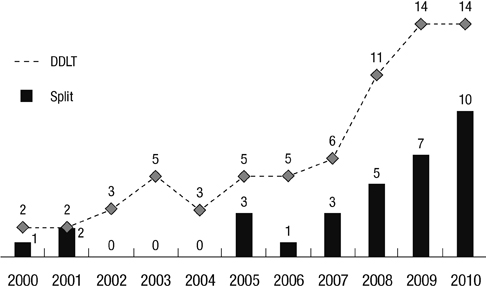
- Pediatric liver transplantation is the standard of care for treatment of liver failure in children. The aim of this study was to identify the characteristics of pediatric liver transplantation in centers located in Korea and determine factors that influence outcomes. This retrospective study was performed using data from between 1988 and 2010 and included all recipients 18 yr old and younger who underwent pediatric liver transplantation in Korea during that period. Our data sources were hospital medical records and the outcome measure was overall patient survival. Univariate and multivariate statistical analyses were undertaken using the Cox proportional hazards model. Five hundred and thirty-four pediatric liver transplantations were performed in 502 children. Median age and average pediatric end-stage liver disease (PELD) score were 20 months and 18 point, respectively. Biliary atresia (57.7%, 308/534) was the most common cause of liver disease. Eighty-two (15.3%) were deceased donor liver transplantations and 454 (84.7%) were living donor liver transplantations. Retransplantation was performed in 32 cases (6%). Overall, 1-, 5-, and 10-yr patient survival rates were 87.8%, 82.2%, and 78.1%, respectively. In multivariate analysis, independent significant predictors of poor patient survival were chronic rejection and retransplantation. This study presents the epidemiologic data for nearly all pediatric liver transplantation in Korea and shows that the independent prognostic factors in patient survival are chronic rejection and retransplantation.
Keyword
MeSH Terms
-
Adolescent
Biliary Atresia/epidemiology
Child
Child, Preschool
End Stage Liver Disease/epidemiology/mortality/*therapy
Female
Graft Survival
Humans
Infant
*Liver Transplantation
Male
Prognosis
Proportional Hazards Models
Republic of Korea
Retrospective Studies
Risk Factors
Severity of Illness Index
Survival Rate
Treatment Outcome
Figure
Cited by 2 articles
-
Pediatric liver transplantation in Korea: long-term outcomes and allocations
Sanghoon Lee, Suk-Koo Lee
Korean J Transplant. 2019;33(1):1-5. doi: 10.4285/jkstn.2019.33.1.1.Pediatric liver transplantation in Korea: long-term outcomes and allocations
Sanghoon Lee, Suk-Koo Lee
J Korean Soc Transplant. 2019;33(1):1-5. doi: 10.4285/jkstn.2019.33.1.1.
Reference
-
1. McDiarmid SV. Current status of liver transplantation in children. Pediatr Clin North Am. 2003. 50:1335–1374.2. Otte JB, de Ville de Goyet J, Reding R, Van Obbergh L, Veyckemans F, Carlier MA, De Kock M, Clement de Clety S, Clapuyt P, Sokal E, et al. Pediatric liver transplantation: from the full-size liver graft to reduced, split, and living related liver transplantation. Pediatr Surg Int. 1998. 13:308–318.3. Starzl TE, Koep LJ, Schroter GP, Halgrimson CG, Porter KA, Weil R 3rd. Liver replacement for pediatric patients. Pediatrics. 1979. 63:825–829.4. Kim KM. Liver transplantation in children. J Korean Pediatr Soc. 2003. 46:736–741.5. Freeman RB Jr, Wiesner RH, Harper A, McDiarmid SV, Lake J, Edwards E, Merion R, Wolfe R, Turcotte J, Teperman L. The new liver allocation system: moving toward evidence-based transplantation policy. Liver Transpl. 2002. 8:851–858.6. Kim MJ, Choe YH. Indication of pediatric liver transplantation. J Korean Soc Transplant. 2011. 25:151–154.7. Ng VL, Fecteau A, Shepherd R, Magee J, Bucuvalas J, Alonso E, McDiarmid S, Cohen G, Anand R. Outcomes of 5-year survivors of pediatric liver transplantation: report on 461 children from a North American Multicenter Registry. Pediatrics. 2008. 122:e1128–e1135.8. McDiarmid SV, Anand R, Martz K, Millis MJ, Mazariegos G. A multivariate analysis of pre-, peri-, and post-transplant factors affecting outcome after pediatric liver transplantation. Ann Surg. 2011. 254:145–154.9. Emre S. Living-donor liver transplantation in children. Pediatr Transplant. 2002. 6:43–46.10. KONOS. access 20 February 2012. Available from: www.konos.go.kr.