Etiology of Invasive Bacterial Infections in Immunocompetent Children in Korea (1996-2005): A Retrospective Multicenter Study
- Affiliations
-
- 1Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea. hoanlee@snu.ac.kr
- 2Department of Pediatrics, School of Medicine, Ewha Womans University, Seoul, Korea.
- 3Department of Pediatrics, College of Medicine, Soonchunhyang University, Seoul, Korea.
- 4Department of Pediatrics, Yonsei University College of Medicine, Severance Children's Hospital, Seoul, Korea.
- 5Department of Pediatrics, Hallym University College of Medicine, Seoul, Korea.
- 6Department of Pediatrics, College of Medicine, Kyunghee University, Seoul, Korea.
- 7Department of Pediatrics, Hanyang University College of Medicine, Seoul, Korea.
- 8Department of Pediatrics, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 9Department of Pediatrics, Korea University College of Medicine, Seoul, Korea.
- 10Department of Pediatrics, Inha University College of Medicine, Incheon, Korea.
- 11Department of Pediatrics, Dankook University College of Medicine, Cheonan, Korea.
- 12Department of Pediatrics, College of Medicine, Pusan National University, Busan, Korea.
- 13Department of Pediatrics, Chonnam National University Medical School, Gwangju, Korea.
- 14Department of Pediatrics, Chonbuk National University Medical School, Jeonju, Korea.
- 15Department of Pediatrics, Yonsei University Wonju College of Medicine, Wonju, Korea.
- KMID: 1782103
- DOI: http://doi.org/10.3346/jkms.2011.26.2.174
Abstract
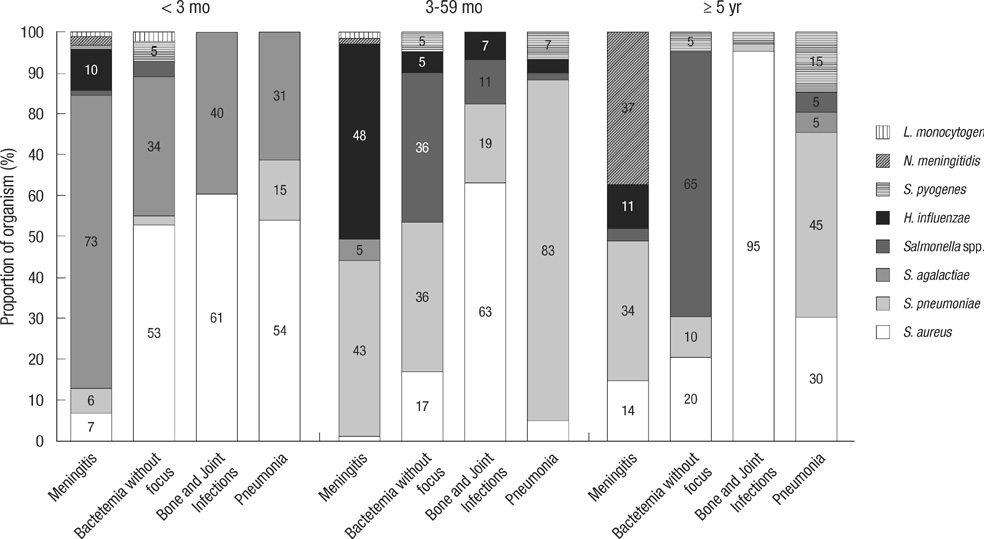
- The purpose of this study was to identify the major etiological agents responsible for invasive bacterial infections in immunocompetent Korean children. We retrospectively surveyed invasive bacterial infections in immunocompetent children caused by eight major pediatric bacteria, namely Streptococcus pneumoniae, Haemophilus influenzae, Neisseria meningitidis, Staphylococcus aureus, Streptococcus agalactiae, Streptococcus pyogenes, Listeria monocytogenes, and Salmonella species that were diagnosed at 18 university hospitals from 1996 to 2005. A total of 768 cases were identified. S. agalactiae (48.1%) and S. aureus (37.2%) were the most common pathogens in infants younger than 3 months. S. agalactiae was a common cause of meningitis (73.0%), bacteremia without localization (34.0%), and arthritis (50%) in this age group. S. pneumoniae (45.3%) and H. influenzae (20.4%) were common in children aged 3 months to 5 yr. S. pneumoniae was a common cause of meningitis (41.6%), bacteremia without localization (40.0%), and bacteremic pneumonia (74.1%) in this age group. S. aureus (50.6%), Salmonella species (16.9%), and S. pneumoniae (16.3%) were common in older children. A significant decline in H. influenzae infections over the last 10 yr was noted. S. agalactiae, S. pneumoniae, and S. aureus are important pathogens responsible for invasive bacterial infections in Korean children.
Keyword
MeSH Terms
Figure
Cited by 10 articles
-
Etiology of Invasive Bacterial Infections in Immunocompetent Children in Korea (2006–2010): a Retrospective Multicenter Study
Kyuyol Rhie, Eun Hwa Choi, Eun Young Cho, Jina Lee, Jin Han Kang, Dong Soo Kim, Yae-Jean Kim, Youngmin Ahn, Byung Wook Eun, Sung Hee Oh, Sung-Ho Cha, Young Jin Hong, Kwang Nam Kim, Nam Hee Kim, Yun-Kyung Kim, Jong-Hyun Kim, Taekjin Lee, Hwang Min Kim, Kun Song Lee, Chun Soo Kim, Su Eun Park, Young Mi Kim, Chi Eun Oh, Sang Hyuk Ma, Dae Sun Jo, Young Youn Choi, Hoan Jong Lee
J Korean Med Sci. 2018;33(6):. doi: 10.3346/jkms.2018.33.e45.Prevalence of group B streptococcus colonization in pregnant women in a tertiary care center in Korea
Da Hyun Kim, Byoung Jin Min, Eun Jung Jung, Jung Mi Byun, Dae Hoon Jeong, Kyung Bok Lee, Moon Su Sung, Ki Tae Kim, Young Nam Kim
Obstet Gynecol Sci. 2018;61(5):575-583. doi: 10.5468/ogs.2018.61.5.575.Trends in Childhood Bacterial Infectious Diseases in the Republic of Korea
Young June Choe, Hoan Jong Lee
Infect Chemother. 2011;43(6):468-473. doi: 10.3947/ic.2011.43.6.468.The Changing Epidemiology of Childhood Pneumococcal Disease in Korea
Young June Choe, Eun Hwa Choi, Hoan Jong Lee
Infect Chemother. 2013;45(2):145-158. doi: 10.3947/ic.2013.45.2.145.Etiology and Clinical Manifestations of Fever in Infants Younger than 3 Months Old: A Single Institution Study, 2008-2010
Joon Young Seok, Ji Eun Kang, Eun Young Cho, Eun Hwa Choi, Hoan Jong Lee
Korean J Pediatr Infect Dis. 2012;19(3):121-130. doi: 10.14776/kjpid.2012.19.3.121.Group B Streptococcal Disease in Korean Neonates
Chi Eun Oh
Korean J Pediatr Infect Dis. 2012;19(2):43-54. doi: 10.14776/kjpid.2012.19.2.43.Serotype Distribution of Invasive Group B Streptococcal Diseases in Infants at Two University Hospitals in Korea
Hye-Kyung Cho, Hye Na Nam, Hye Jung Cho, Dong Woo Son, Yong Kyun Cho, Yiel-Hea Seo, Yae-Jean Kim, Byung Wook Eun
Pediatr Infect Vaccine. 2017;24(2):79-86. doi: 10.14776/piv.2017.24.2.79.Cerebral Venous Sinus Thrombosis with Meningitis and Septicemia due to Haemophilus influenzae Type f in an Immunocompetent Child
HyungKyu Han, Kyung Jae Lee, Hee Joon Yu
Pediatr Infect Vaccine. 2019;26(3):188-193. doi: 10.14776/piv.2019.26.e19.Clinical Manifestations of Invasive Infections due to
Streptococcus pyogenes in Children
Nuri Yang, Hyeon Seung Lee, Jae Hong Choi, Eun Young Cho, Eun Hwa Choi, Hoan Jong Lee, Hyunju Lee
Korean J Pediatr Infect Dis. 2014;21(2):129-138. doi: 10.14776/kjpid.2014.21.2.129.Epidemiology of
Staphylococcus aureus Bacteremia in Children at a Single Center from 2002 to 2016
Seonhee Lim, Seok Gyun Ha, Hann Tchah, In Sang Jeon, Eell Ryoo, Dong Woo Son, Hye Jung Cho, Yong Han Sun, Hyo Jung Kim, Jung Min Ahn, Hye-Kyung Cho
Pediatr Infect Vaccine. 2019;26(1):11-21. doi: 10.14776/piv.2019.26.1.11.
Reference
-
1. McCracken GH Jr. Group B streptococci: the new challenge in neonatal infections. J Pediatr. 1973. 82:703–706.2. Schuchat A, Hilger T, Zell E, Farley MM, Reingold A, Harrison L, Lefkowitz L, Danila R, Stefonek K, Barrett N, Morse D, Pinner R. Active Bacterial Core Surveillance Team of the Emerging Infections Program Network. Active bacterial core surveillance of the emerging infections program network. Emerg Infect Dis. 2001. 7:92–99.3. Adams WG, Deaver KA, Cochi SL, Plikaytis BD, Zell ER, Broome CV, Wenger JD. Decline of childhood Haemophilus influenzae type b (Hib) disease in the Hib vaccine era. JAMA. 1993. 269:221–226.4. Hsu K, Pelton S, Karumuri S, Heisey-Grove D, Klein J. Massachusetts Department of Public Health Epidemiologists. Population-based surveillance for childhood invasive pneumococcal disease in the era of conjugate vaccine. Pediatr Infect Dis J. 2005. 24:17–23.5. Kim JS, Jang YT, Kim JD, Park TH, Park JM, Kilgore PE, Kennedy WA, Park E, Nyambat B, Kim DR, Hwang PH, Kim SJ, Eun SH, Lee HS, Cho JH, Kim YS, Chang SJ, Huang HF, Clemens JD, Ward JI. Incidence of Haemophilus influenzae type b and other invasive diseases in South Korean children. Vaccine. 2004. 22:3952–3962.6. Shin S, Shin YJ, Ki M. Cost-benefit analysis of Haemophilus influenzae type B immunization in Korea. J Korean Med Sci. 2008. 23:176–184.7. Choi E. Direct and indirect effects of pneumococcal protein conjugate vaccine. J Korean Med Assoc. 2008. 51:119–126.8. Korean statistical information service. KOSIS. accessed on 18 Aug 2010. Available at http://kosis.kr/nsportal/index/index.jsp.9. Saarinen M, Takala AK, Koskenniemi E, Kela E, Rönnberg PR, Pekkanen E, Kiiski P, Eskola J. Finnish Pediatric Invasive Infection Study Group. Spectrum of 2,836 cases of invasive bacterial or fungal infections in children: results of prospective nationwide five-year surveillance in Finland. Clin Infect Dis. 1995. 21:1134–1144.10. Nam SG, Lee HJ. Etiology of invasive bacterial infections in apparently healthy children. Korean J Infect Dis. 1998. 30:227–234.11. Lee JH, Song EK, Lee JA, Kim NH, Kim DH, Park KW, Choi EH, Lee HJ. Clinical entities and etiology of invasive bacterial infections in apparently healthy children. Korean J Pediatr. 2005. 48:1193–1200.12. Stoll BJ. Kligman RM, Behrman RE, Jenson HB, Stanton BF, editors. Infections of the neonatal infant. Nelson textbook of pediatrics. 2007. 18th ed. Philadelphia: Elsevier Saunders;794–811.13. Kim KA, Shin SM, Choi JH. A nationwide survey on the causative organisms of neonatal sepsis in Korea. J Korean Pediatr Soc. 2002. 45:55–63.14. Moon JH, Oh SH, Kim HW, Moon SJ, Choi TY. Neonatal sepsis and antimicrobial susceptibilities in the neonatal intensive care unit and nursery. Korean J Pediatr Infect Dis. 2002. 9:163–174.15. Ammerlaan HS, Kluytmans JA, Wertheim HF, Nouwen JL, Bonten MJ. Eradication of methicillin-resistant Staphylococcus aureus carriage: a systematic review. Clin Infect Dis. 2009. 48:922–930.16. Lee JH, Park JJ, Sung IK, Lee BC. Clinical observation in 40 cases with neonatal sepsis. J Korean Pediatr Soc. 1990. 33:1489–1494.17. Suryati BA, Watson M. Staphylococcus aureus bacteraemia in children: a 5-year retrospective review. J Paediatr Child Health. 2002. 38:290–294.18. Sattler CA, Correa AG. Feigin RD, Cherry JD, Demmler GJ, Kaplan SL, editors. Coagulase-positive staphylococcal infections (Staphylococcus aureus). Textbook of pediatric infectious diseases. 2004. 5th ed. Philadelphia: Elsevier Saunders;1099–1129.19. Lowy FD. Staphylococcus aureus infections. N Engl J Med. 1998. 339:520–532.20. Centers for Disease Control and Prevention (CDC). Perinatal group B streptococcal disease after universal screening recommendations-United States, 2003-2005. MMWR Morb Mortal Wkly Rep. 2007. 56:701–705.21. Jang GC, Shin KM, Yong DE, Lee KW, Kim DS. Changing patterns of antibiotic-resistant rates and clinical features in pneumococcal infections. Korean J Pediatr Infect Dis. 2003. 10:81–86.22. Active Bacterial Core Surveillance Report, Emerging Infections Program Network, Streptococcus pneumoniae, 1999. Centers for Disease Control and Prevention. accessed on 18 Aug 2010. Available at http://www.cdc.gov/abcs/survreports/spneu99.pdf.23. Active Bacterial Core Surveillance Report, Emerging Infections Program Network, Streptococcus pneumoniae, 2005. Centers for Disease Control and Prevention. accessed on 18 Aug 2010. Available at http://www.cdc.gov/abcs/survreports/spneu05.pdf.24. Lee HJ. Epidemiology of systemic Haemophilus influenzae disease in Korean children. Pediatr Infect Dis J. 1998. 17:9 Suppl. S185–S189.25. Peltola H. Worldwide Haemophilus influenzae type b disease at the beginning of the 21st century: global analysis of the disease burden 25 years after the use of the polysaccharide vaccine and a decade after the advent of conjugates. Clin Microbiol Rev. 2000. 13:302–317.26. Yagupsky P, Maimon N, Dagan R. Increasing incidence of nontyphi Salmonella bacteremia among children living in southern Israel. Int J Infect Dis. 2002. 6:94–97.27. Ispahani P, Slack RC. Enteric fever and other extraintestinal salmonellosis in University Hospital, Nottingham, UK, between 1980 and 1997. Eur J Clin Microbiol Infect Dis. 2000. 19:679–687.28. Vugia DJ, Samuel M, Farley MM, Marcus R, Shiferaw B, Shallow S, Smith K, Angulo FJ. Emerging Infections Program FoodNet Working Group. Invasive Salmonella infections in the United States, FoodNet, 1996-1999: incidence, serotype distribution, and outcome. Clin Infect Dis. 2004. 38:Suppl 3. S149–S156.29. Arditi M, Mason EO Jr, Bradley JS, Tan TQ, Barson WJ, Schutze GE, Wald ER, Givner LB, Kim KS, Yogev R, Kaplan SL. Three-year multicenter surveillance of pneumococcal meningitis in children: clinical characteristics, and outcome related to penicillin susceptibility and dexamethasone use. Pediatrics. 1998. 102:1087–1097.30. Alpern ER, Alessandrini EA, Bell LM, Shaw KN, McGowan KL. Occult bacteremia from a pediatric emergency department: current prevalence, time to detection, and outcome. Pediatrics. 2000. 106:505–511.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Entities and Etiology of Invasive Bacterial Infections in Apparently Healthy Children
- Etiology of Invasive Bacterial Infections in Immunocompetent Children in Korea (1996-2005): A Retrospective Multicenter Study
- Etiology of Invasive Bacterial Infections in Apparently Healthy Children
- The Causative Organisms of Pediatric Bacterial Meningitis: A Single Center Experience from 1996 to 2005
- Etiology of Invasive Bacterial Infections in Immunocompetent Children in Korea (2006–2010): a Retrospective Multicenter Study