The Causative Organisms of Bacterial Meningitis in Korean Children in 1996-2005
- Affiliations
-
- 1Department of Pediatrics, School of Medicine, Ewha Womans University, Seoul, Korea. kaykim@ewha.ac.kr
- 2Department of Pediatrics, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 3Department of Pediatrics, College of Medicine, Hallym University, Seoul, Korea.
- 4Department of Pediatrics, Yonsei University College of Medicine, Seoul, Korea.
- 5Department of Pediatrics, College of Medicine, Korea University, Ansan, Korea.
- 6Department of Pediatrics, Chonbuk National University, College of Medicine, Jeonju, Korea.
- 7Department of Pediatrics, College of Medicine, Soonchunhyang University, Bucheon, Korea.
- 8Department of Pediatrics, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 9Department of Pediatrics, School of Medicine, Busan National University, Busan, Korea.
- 10Department of Pediatrics, Hanyang University College of Medicine, Seoul, Korea.
- 11Department of Pediatrics, Dankook University College of Medicine, Cheonan, Korea.
- 12Department of Pediatrics, Kyunghee University School of Medicine, Seoul, Korea.
- 13Department of Pediatrics, Chonnam National University Medical School, Gwangju, Korea.
- 14Department of Pediatrics, Inha University College of Medicine, Incheon, Korea.
- 15Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2150869
- DOI: http://doi.org/10.3346/jkms.2010.25.6.895
Abstract
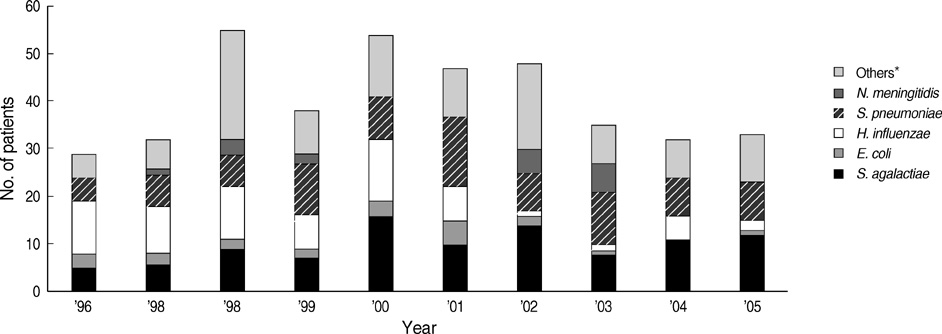
- Bacterial meningitis remains a serious cause of morbidity and mortality in childhood, despite the availability of effective vaccines against Haemophilus influenzae type b (Hib) or Streptococcus pneumoniae. The purpose of this study was to analyze data on bacterial meningitis cases in Korea from 1996 through 2005. The information of all hospitalized bacteria-proven meningitis cases was obtained from 17 university hospitals nationwide. A total of 402 cases were identified. Of these, 125 (29.9%) cases were neonates. Streptococcus agalactiae was the most common bacteria responsible for 99 (24.6%) of all cases regardless of age, followed by S. pneumoniae for 91 (22.6%) and H. influenzae for 67 (16.7%) patients. The common etiology beyond the neonatal period was S. pneumoniae for 91 (33.0%) followed by H. influenzae for 63 (22.8%) patients. The overall case fatality rate was 9.4%, which was similar with that in 1986-1995. In conclusion, S. agalactiae, S. pneumoniae and H. influenzae were important etiologic agents of bacterial meningitis in children in the last 10 yrs. It is required to establish the preventive strategy of the three bacteria. The nationwide epidemiologic study should be continued to evaluate immunization strategy and efficacy.
Keyword
Figure
Cited by 9 articles
-
Clinical Practice Guidelines for the Management of Bacterial Meningitis in Adults in Korea
, , , ,
Infect Chemother. 2012;44(3):140-163. doi: 10.3947/ic.2012.44.3.140.The Changing Epidemiology of Childhood Pneumococcal Disease in Korea
Young June Choe, Eun Hwa Choi, Hoan Jong Lee
Infect Chemother. 2013;45(2):145-158. doi: 10.3947/ic.2013.45.2.145.Revised Adult Immunization Guideline Recommended by the Korean Society of Infectious Diseases, 2014
Won Suk Choi, Jung-Hyun Choi, Ki Tae Kwon, Kyung Seo, Min A Kim, Sang-Oh Lee, Young Jin Hong, Jin-Soo Lee, Joon Young Song, Ji Hwan Bang, Hee-Jung Choi, Young-Hwa Choi, Dong Gun Lee, Hee Jin Cheong, ,
Infect Chemother. 2015;47(1):68-79. doi: 10.3947/ic.2015.47.1.68.Group B Streptococcal Disease in Korean Neonates
Chi Eun Oh
Korean J Pediatr Infect Dis. 2012;19(2):43-54. doi: 10.14776/kjpid.2012.19.2.43.Meningococcal Disease and Quadrivalent MenACWY-CRM Vaccine (Menveo®)
Theodore F. Tsai
Korean J Pediatr Infect Dis. 2012;19(3):89-110. doi: 10.14776/kjpid.2012.19.3.89.Serotype Distribution of Invasive Group B Streptococcal Diseases in Infants at Two University Hospitals in Korea
Hye-Kyung Cho, Hye Na Nam, Hye Jung Cho, Dong Woo Son, Yong Kyun Cho, Yiel-Hea Seo, Yae-Jean Kim, Byung Wook Eun
Pediatr Infect Vaccine. 2017;24(2):79-86. doi: 10.14776/piv.2017.24.2.79.Cerebral Venous Sinus Thrombosis with Meningitis and Septicemia due to Haemophilus influenzae Type f in an Immunocompetent Child
HyungKyu Han, Kyung Jae Lee, Hee Joon Yu
Pediatr Infect Vaccine. 2019;26(3):188-193. doi: 10.14776/piv.2019.26.e19.Trend of Bacteria and Fungi Isolated from Cerebrospinal Fluid Culture in a Tertiary Care Hospital During Recent Two Decades (1997–2016)
Su Geun Lee, Minwoo Kim, Gyu Yel Hwang, Gilsung Yoo, Young Uh
Ann Clin Microbiol. 2017;20(4):81-89. doi: 10.5145/ACM.2017.20.4.81.Late-Onset Group B Streptococcal Meningitis Complicated with Extensive Cerebral Infarction
Min Su Cho, Yongmin Kim, Hye-Kyung Cho, Soo-Han Choi
Pediatr Infect Vaccine. 2018;25(1):45-49. doi: 10.14776/piv.2018.25.1.45.
Reference
-
1. Centers for Disease Control and Prevention (CDC). Trends in perinatal group B streptococcal disease-United States, 2000-2006. MMWR Morb Mortal Wkly Rep. 2009. 58:109–112.2. Fluegge K, Siedler A, Heinrich B, Schulte-Moenting J, Moennig MJ, Bartels DB, Dammann O, von Kries R, Berner R. German Pediatric Surveillance Unit Study Group. Incidence and clinical presentation of invasive neonatal group B streptococcal infections in Germany. Pediatrics. 2006. 117:e1139–e1145.
Article3. Sáez-Llorens X, McCracken GH Jr. Bacterial meningitis in children. Lancet. 2003. 361:2139–2148.
Article4. Chávez-Bueno S, McCracken GH Jr. Bacterial meningitis in children. Pediatr Clin North Am. 2005. 52:795–810.
Article5. Kim KH, Sohn YM, Kang JH, Kim KN, Kim DS, Kim JH, Kim CH, Shin YK, Oh SH, Lee HJ, Cha SH, Hong YJ, Sohn KC. The causative organisms of bacterial meningitis in Korean children, 1986-1995. J Korean Med Sci. 1998. 13:60–64.
Article6. Kim KH, Lee H, Chung EH, Kang JH, Kim JH, Kim JS, Lee HJ, Oh SH, Park EA, Park SE. Immunogenicity and safety of two different Haemophilus influenzae type b conjugate vaccines in Korean infants. J Korean Med Sci. 2008. 23:929–936.
Article7. Cowgill KD, Ndiritu M, Nyiro J, Slack MP, Chiphatsi S, Ismail A, Kamau T, Mwangi I, English M, Newton CR, Feikin DR, Scott JA. Effectiveness of Haemophilus influenzae type b Conjugate vaccine introduction into routine childhood immunization in Kenya. JAMA. 2006. 296:671–678.
Article8. Adegbola RA, Secka O, Lahai G, Lloyd-Evans N, Njie A, Usen S, Oluwalana C, Obaro S, Weber M, Corrah T, Mulholland K, McAdam K, Greenwood B, Milligan PJ. Elimination of Haemophilus influenzae type b (Hib) disease from The Gambia after the introduction of routine immunisation with a Hib conjugate vaccine: a prospective study. Lancet. 2005. 366:144–150.
Article9. Lee YJ, Lee SJ, Park HJ, Lee YH, Kang SY, Kim YC, Lee IK, Lee KY, Lee KS, Kim WS. A clinical study of child bacterial meningitis in Daejeon and Chungcheong area: 2001-2005. Korean J Pediatr. 2007. 50:157–162.
Article10. Kim HJ, Lee JW, Lee KY, Lee HS, Hong JH, Hahn SH, Whang KT. Causative organisms in children with bacterial meningitis (1992-2002). J Korean Pediatr Soc. 2003. 46:1085–1088.11. Sáez-Llorens X, McCracken GH Jr. Antimicrobial and anti-inflammatory treatment of bacterial meningitis. Infect Dis Clin North Am. 1999. 13:619–636.12. Schuchat A, Robinson K, Wenger JD, Harrison LH, Farley M, Reingold AL, Lefkowitz L, Perkins BA. Bacterial meningitis in the United States in 1995. Active Surveillance Team. N Engl J Med. 1997. 337:970–976.13. Phares CR, Lynfield R, Farley MM, Mohle-Boetani J, Harrison LH, Petit S, Craig AS, Schaffner W, Zansky SM, Gershman K, Stefonek KR, Albanese BA, Zell ER, Schuchat A, Schrag SJ. Epidemiology of invasive group B streptococcal disease in the United States, 1999-2005. JAMA. 2008. 299:2056–2065.14. López Sastre JB, Fernández Colomer B, Coto Cotallo GD, Ramos Aparicio A. Grupo de Hospitales Castrillo. Trends in the epidemiology of neonatal sepsis of vertical transmission in the era of group B streptococcal prevention. Acta Paediatr. 2005. 94:451–457.15. Mendsaikhan J, Watt JP, Mansoor O, Suvdmaa N, Edmond K, Litt DJ, Nymadawa P, Baoping Y, Altantsetseg D, Slack M. Childhood bacterial meningitis in Ulaanbaatar, Mongolia, 2002-2004. Clin Infect Dis. 2009. 48:Suppl 2. S141–S146.16. Kalies H, Siedler A, Gröndahl B, Grote V, Milde-Busch A, von Kries R. Invasive Haemophilus influenzae infections in Germany: impact of non-type b serotypes in the post-vaccine era. BMC Infect Dis. 2009. 9:45.17. Lewis RF, Kisakye A, Gessner BD, Duku C, Odipio JB, Iriso R, Nansera D, Braka F, Makumbi I, Kekitiinwa A. Action for child survival: elimination of Haemophilus influenzae type b meningitis in Uganda. Bull World Health Organ. 2008. 86:292–301.18. Kelly DF, Moxon ER, Pollard AJ. Haemophilus influenzae type b conjugate vaccines. Immunology. 2004. 113:163–174.19. World Health Organization. WHO position paper on Haemophilus influenzae type b conjugate vaccines. Wkly Epidemiol Rec. 2006. 81:445–452.20. Nigrovic LE, Kuppermann N, Malley R. Bacterial Meningitis Study Group of the Pediatric Emergency Medicine Collaborative Research Committee of the American Academy of Pediatrics. Children with bacterial meningitis presenting to the emergency department during the pneumococcal conjugate vaccine era. Acad Emerg Med. 2008. 15:522–528.21. Neuman HB, Wald ER. Bacterial meningitis in childhood at the Children's Hospital of Pittsburgh: 1988-1998. Clin Pediatr (Phila). 2001. 40:595–600.22. Centers for Disease Control and Prevention (CDC). Pediatric bacterial meningitis surveillance-African region, 2002-2008. MMWR Morb Mortal Wkly Rep. 2009. 58:493–497.23. Giorgi Rossi P, Mantovani J, Ferroni E, Forcina A, Stanghellini E, Curtale F, Borgia P. Incidence of bacterial meningitis (2001-2005) in Lazio, Italy: the results of a integrated surveillance system. BMC Infect Dis. 2009. 9:13.24. Theodoridou MN, Vasilopoulou VA, Atsali EE, Pangalis AM, Mostrou GJ, Syriopoulou VP, Hadjichristodoulou CS. Meningitis registry of hospitalized cases in children: epidemiological patterns of acute bacterial meningitis throughout a 32-year period. BMC Infect Dis. 2007. 7:101.25. Campagne G, Schuchat A, Djibo S, Ousséini A, Cissé L, Chippaux JP. Epidemiology of bacterial meningitis in Niamey, Niger, 1981-96. Bull World Health Org. 1999. 77:499–508.26. Hsu HE, Shutt KA, Moore MR, Beall BW, Bennett NM, Craig AS, Farley MM, Jorgensen JH, Lexau CA, Petit S, Reingold A, Schaffner W, Thomas A, Whitney CG, Harrison LH. Effect of pneumococcal conjugate vaccine on pneumococcal meningitis. N Engl J Med. 2009. 360:244–256.27. Choi EH, Kim SH, Eun BW, Kim SJ, Kim NH, Lee J, Lee HJ. Streptococcus pneumoniae serotype 19A in children, South Korea. Emerg Infect Dis. 2008. 14:275–281.28. Husain EH, Al-Shawaf F, Bahbahani E, El-Nabi MH, Al-Fotooh KA, Shafiq MH, Al-Ateeqi N, Abo Talib MA. Epidemiology of childhood meningitis in Kuwait. Med Sci Monit. 2007. 13:CR220–CR223.29. Baraff LJ, Lee SI, Schriger DL. Outcomes of bacterial meningitis in children: a meta-analysis. Pediatr Infect Dis J. 1993. 12:389–394.30. Grandgirard D, Leib SL. Strategies to prevent neuronal damage in paediatric bacterial meningitis. Curr Opin Pediatr. 2006. 18:112–118.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Causative Organisms of Pediatric Bacterial Meningitis: A Single Center Experience from 1996 to 2005
- Acute Bacterial Meningitis: Causative Organisms, Clinical Characteristics and Prognosis
- The Causative Organisms of Neonatal and Pediatric Bacterial Meningitis in Korea(2000~2005)
- Causative Organisms in Children with Bacterial Meningitis(1992-2002)
- Bacterial Meningitis in Children in One Tertiary Hospital