Korean Circ J.
2010 Jun;40(6):266-271. 10.4070/kcj.2010.40.6.266.
The Correlation Between Left Ventricular Failure and Right Ventricular Systolic Dysfunction Occurring in Thyrotoxicosis
- Affiliations
-
- 1Department of Internal Medicine, Hallym University College of Medicine, Seoul, Korea. dgpark@hallym.or.kr
- KMID: 2225186
- DOI: http://doi.org/10.4070/kcj.2010.40.6.266
Abstract
- BACKGROUND AND OBJECTIVES
Heart failure rarely occurs in patients with thyrotoxicosis (6%), with half of the cases having left ventricular dysfunction (LVD). Although a few studies reported isolated right heart failure in thyrotoxicosis, there has been no evaluation of relationship between LVD and right ventricular dysfunction (RVD).
SUBJECTS AND METHODS
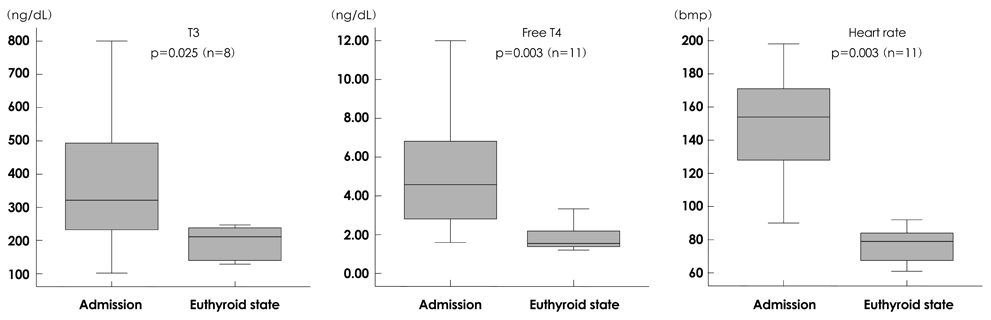
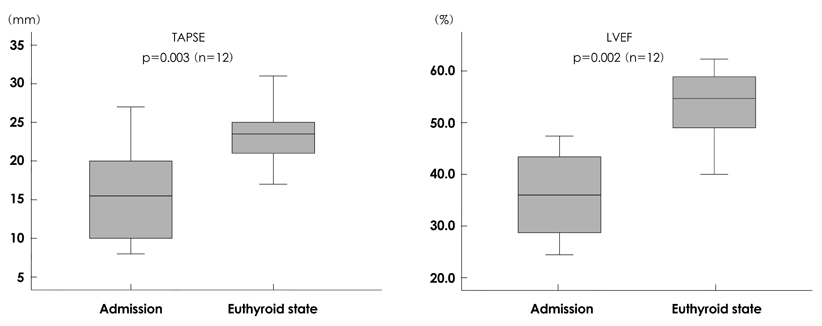
We enrolled 12 patients (mean age: 51+/-11 years, 9 females) diagnosed as having thyrotoxicosis with heart failure and LVD {left ventricular ejection fraction (LVEF) <40%}, and divided them into two groups {Group I with RVD defined as tricuspid annular plane excursion (TAPSE) less than 15 mm and Group II without RVD}. Clinical features, laboratory variables, and echocardiographic parameters were compared between two groups.
RESULTS
RVD was found in 6 (50%) patients. On admission, there were no significant differences between the two groups in clinical features, laboratory variables, or echocardiographic parameters including atrial fibrillation {6 vs. 5, not significant (NS)}, heart rate (149+/-38 vs. 148+/-32/min, NS), LVEF (36.7+/-9.5 vs. 35.1+/-6.3%, NS), or the tricuspid regurgitation peak pressure gradient (TRPPG, 30.9+/-2.0 vs. 36.3+/-9.3 mmHg, NS). After antithyroid treatment, all achieved an euthyroid state and both ventricular functions were recovered. All data, including the recovery time of LVEF and the change of heart rate between two groups, displayed no significant differences.
CONCLUSION
In half of patients, RVD was combined with thyrotoxicosis-associated LVD. There were no differences in clinical factors or hemodynamic parameters between patients with and without RVD. This suggests that RVD is not secondary to thyrotoxicosis-associated LVD.
MeSH Terms
Figure
Cited by 2 articles
-
A Rapid Improvement of Heart Failure after Treatment of Hyperthyroidism
Ki Jeong Park, Myung Ho Jeong, Min Suk Kim, Soo Young Jang, Ki Hong Lee, Min Goo Lee, Keun-Ho Park, Doo Sun Sim, Nam Sik Yoon, Hyun Ju Yoon, Kye Hun Kim, Young Joon Hong, Ju Han Kim, Youngkeun Ahn, Jeong Gwan Cho, Jong Chun Park, Jung Chae Kang
J Lipid Atheroscler. 2012;1(2):101-104. doi: 10.12997/jla.2012.1.2.101.The Effect of Tonsillectomy and Adenoidectomy on Right Ventricle Function and Pulmonary Artery Pressure by Using Doppler Echocardiography in Children
Onur Çağlar Acar, Abdurrahman Üner, Mehmet Fatih Garça, İbrahim Ece, Serdar Epçaçan, Mahfuz Turan, Ferhat Kalkan
Clin Exp Otorhinolaryngol. 2016;9(2):163-167. doi: 10.21053/ceo.2015.00087.
Reference
-
1. Dahl P, Danzi S, Kein I. Thyrotoxic cardiac disease. Curr Heart Fail Rep. 2008. 5:170–176.2. Klein I, Ojamaa K. Thyroid hormone and the cardiovascular system. N Engl J Med. 2001. 344:501–509.3. Umana E, Solares CA, Alpert MA. Tachycardia-induced cardiomyopathy. Am J Med. 2003. 114:51–55.4. Siu CW, Yeung CY, Lau CP, Kung A, Tse HF. Incidence, clinical characteristics and outcome of congestive heart failure as the initial presentation in patients with primary hyperthyroidism. Heart. 2007. 93:483–487.5. Di Giovambattista R. Hyperthyroidism as a reversible cause of right ventricular overload and congestive heart failure. Cardiovasc Ultrasound. 2008. 6:29.6. Lozano HF, Sharma CN. Reversible pulmonary hypertension, tricuspid regurgitation and right-sided heart failure associated with hyperthyroidism: case report and review of the literature. Cardiol Rev. 2004. 12:299–305.7. Cohen J, Schattner A. Right heart failure and hyperthyroidism: a neglected presentation. Am J Med. 2003. 115:76–77.8. Park JH, Shong MH, Lee JH, Choi SW, Jeoung JO, Seong IW. Reversible severe tricuspid regurgitation with right heart failure associated with thyrotoxicosis. Thyroid. 2006. 16:813–814.9. Lozano HF, Sharma CN. Reversible pulmonary hypertension, tricuspid regurgitation and right-sided heart failure associated hyperthyroidism: case report and review of the literature. Cardiol Rev. 2004. 12:299–305.10. Nakchbandi I, Wirth J, Inzucchi S. Pulmonary hypertension caused by Graves' thyrotoxicosis: normal pulmonary hemodynamics restored by (131)I treatment. Chest. 1999. 116:1483–1485.11. Syrius V, Plastiras SC, Paterakis T, Moyssakis I, Vlachoyiannopoulos P. Severe reversible right heart failure in a patient with hyperthyroidism. Int J Clin Pract. 2008. 62:334–336.12. Kang B, Cho DK, Byun KH, Eun LY, Cho YH. Isolated pulmonary arterial hypertension-Janus' faces of hyperthyroidism. Korean Circ J. 2009. 39:168–170.13. Pereira N, Parisi A, Dec GW, Choo J, Hajjar R, Gordon PC. Myocardial stunning in hyperthyroidism. Clin Cardiol. 2000. 23:298–300.14. Kwak JJ, Choi YJ, Kwon KH, Park SH. A case of myocardial stunning in hyperthyroidism. Korean Circ J. 2004. 34:516–519.15. Kiss E, Jakab G, Kranias EG, Edes I. Thyroid hormone-induced alterations in phospholamban protein expression: regulatory effects on sarcoplasmic reticulum Ca2+ transport and myocardial relaxation. Circ Res. 1994. 75:245–251.16. Garcia-Gonzalez MJ, Dominguez-Rodriguez A, Garcia CR. Acute right ventricular dysfunction after cardioversion or hyperthyroid cardiomyopathy in an unrecognized thyrotoxicosis patient? Am J Emerg Med. 2007. 25:723–724.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Correlation Between Left Ventricular Failure and Right Ventricular Systolic Dysfunction Occurring in Thyrotoxicosis
- Left Ventricular Diastolic Functions by M-Mode Echocardiogram in Essential Hypertensive Patients
- Acute Heart Failure after Relief of Massive Pericardial Effusion
- Transient Left Ventricular Systolic Dysfunction Associated with Carbon Monoxide Toxicity
- A Rapid Improvement of Heart Failure after Treatment of Hyperthyroidism