The Effects of Postoperative Brachial Plexus Block Using MgSO4 on the Postoperative Pain after Upper Extremity Surgery
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Kwandong University College of Medicine, Goyang, Korea. aerina1224@naver.com
- KMID: 2278105
- DOI: http://doi.org/10.3344/kjp.2011.24.3.158
Abstract
- BACKGROUND
Although a brachial plexus block can be used to provide anesthesia and analgesia for upper extremity surgery, its effects using MgSO4 on postoperative pain management have not been reported. The aim of this study was to evaluate brachial plexus block using MgSO4 on postoperative analgesia.
METHODS
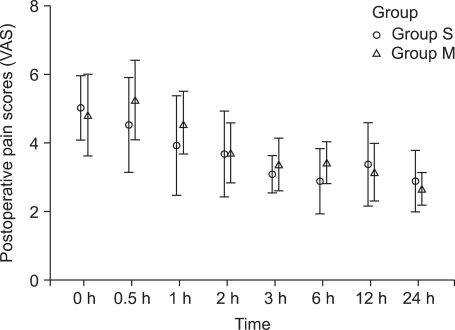
Thirty-eight patients who were scheduled to undergo upper extremity surgery were randomly allocated into two groups: patients receiving axillary brachial plexus block with 0.2% ropivacaine 20 ml and normal saline 2 ml (group S) or 0.2% ropivacaine 20 ml and MgSO4 200 mg (group M). Before extubation, the blocks were done and patient controlled analgesia was started, and then, the patients were transported to a postanesthetic care unit. The postoperative visual analogue scale (VAS), opioid consumption, and side effects were recorded.
RESULTS
The two groups were similar regarding the demographic variables and the duration of the surgery. No differences in VAS scores were observed between the two groups. There was no statistically significant difference in opioid consumption between the two groups. Nausea was observed in three patients for each group.
CONCLUSIONS
Axillary brachial plexus block using MgSO4 did not reduce the level of postoperative pain and opioid consumption.
Keyword
MeSH Terms
Figure
Cited by 4 articles
-
Ultrasound-Guided Axillary Brachial Plexus Block Performed by OIrthopedic Surgeon for Distal Radius Fracture Surgery
Doohoon Sun, Chul-Hyung Lee, Cheol-U Kim, Deukhee Jung, Chung-Han An
Arch Hand Microsurg. 2019;24(2):152-161. doi: 10.12790/ahm.2019.24.2.152.Ultrasound-Guided Axillary Brachial Plexus Block, Performed by Orthopedic Surgeons
Cheol-U Kim, Chul-Hyung Lee, Ja-Yeong Yoon, Seung-Koo Rhee
J Korean Orthop Assoc. 2018;53(6):513-521. doi: 10.4055/jkoa.2018.53.6.513.The Efficacy of Ultrasound-Guided Brachial Plexus Block in Trauma Patients
Jung Ho Rah, Sung Min Kwon, Jae Hak Cha, Jun Pyo Lee, Jae Hyun Kim
J Korean Soc Surg Hand. 2014;19(1):13-18. doi: 10.12790/jkssh.2014.19.1.13.Feasibility of Early and Repeated Low-dose Interscalene Brachial Plexus Block for Residual Pain in Acute Cervical Radiculopathy Treated with NSAIDS
Toshio Iwata, Mari Mitoro, Naoya Kuzumoto
Korean J Pain. 2014;27(2):125-132. doi: 10.3344/kjp.2014.27.2.125.
Reference
-
1. Junger A, Klasen J, Benson M, Sciuk G, Hartmann B, Sticher J, et al. Factors determining length of stay of surgical day-case patients. Eur J Anaesthesiol. 2001; 18:314–321. PMID: 11350474.
Article2. Karakaya D, Büyükgöz F, Bariş S, Güldoğuş F, Tür A. Addition of fentanyl to bupivacaine prolongs anesthesia and analgesia in axillary brachial plexus block. Reg Anesth Pain Med. 2001; 26:434–438. PMID: 11561263.
Article3. Jamnig D, Kapral S, Urak G, Lehofer F, Likar R, Trampitsch E, et al. Addition of fentanyl to mepivacaine does not affect the duration of brachial plexus block. Acute Pain. 2003; 5:51–56.
Article4. Reuben SS, Reuben JP. Brachial plexus anesthesia with verapamil and/or morphine. Anesth Analg. 2000; 91:379–383. PMID: 10910852.
Article5. Gormley WP, Murray JM, Fee JP, Bower S. Effect of the addition of alfentanil to lignocaine during axillary brachial plexus anaesthesia. Br J Anaesth. 1996; 76:802–805. PMID: 8679353.
Article6. Kim TH. Clonidine added to lidocaine prolongs the duration of anesthesia and analgesia during brachial plexus block. J Korean Pain Soc. 2001; 14:41–45.7. Lee HS. Comparison of adding clonidine versus epinephrine into local anesthetics in brachial plexus block. J Korean Pain Soc. 1994; 7:205–210.8. Yang JH, Lee JJ, Hwang SM, Lim SY. The effect of fentanyl or epinephrine addition to ropivacaine in brachial plexus block. Korean J Anesthesiol. 2004; 47:655–659.
Article9. Lee KY, Shim KD, Shim YH, Noh JS, Kang WC, Lee JS. Comparison between a fentanyl and clonidine admixture to lidocaine in a brachial plexus block. Korean J Anesthesiol. 2003; 44:500–506.
Article10. Lee IH, Lee IO, Kong MH, Lee MK, Kim NS, Choi YS, et al. Clinical effects of ketamine on ropivacaine in brachial plexus blockade. Korean J Anesthesiol. 2001; 40:721–727.
Article11. Kim DH, Sohn BK. The effect of clonidine added to lidocaine on the duration of anesthesia and analgesia after brachial plexus block. Korean J Anesthesiol. 1998; 35:479–483.
Article12. Telci L, Esen F, Akcora D, Erden T, Canbolat AT, Akpir K. Evaluation of effects of magnesium sulphate in reducing intraoperative anaesthetic requirements. Br J Anaesth. 2002; 89:594–598. PMID: 12393361.
Article13. Singelyn FJ, Dangoisse M, Bartholomée S, Gouverneur JM. Adding clonidine to mepivacaine prolongs the duration of anesthesia and analgesia after axillary brachial plexus block. Reg Anesth. 1992; 17:148–150. PMID: 1606097.14. Kapral S, Gollmann G, Waltl B, Likar R, Sladen RN, Weinstabl C, et al. Tramadol added to mepivacaine prolongs the duration of an axillary brachial plexus blockade. Anesth Analg. 1999; 88:853–856. PMID: 10195537.
Article15. Dubé L, Granry JC. The therapeutic use of magnesium in anesthesiology, intensive care and emergency medicine: a review. Can J Anaesth. 2003; 50:732–746. PMID: 12944451.
Article16. Fawcett WJ, Haxby EJ, Male DA. Magnesium: physiology and pharmacology. Br J Anaesth. 1999; 83:302–320. PMID: 10618948.
Article17. Schulz-Stübner S, Wettmann G, Reyle-Hahn SM, Rossaint R. Magnesium as part of balanced general anaesthesia with propofol, remifentanil and mivacurium: a double-blind, randomized prospective study in 50 patients. Eur J Anaesthesiol. 2001; 18:723–729. PMID: 11580778.
Article18. McQuay HJ, Dickenson AH. Implications of nervous system plasticity for pain management. Anaesthesia. 1990; 45:101–102. PMID: 2157345.
Article19. Woolf CJ, Chong MS. Preemptive analgesia--treating postoperative pain by preventing the establishment of central sensitization. Anesth Analg. 1993; 77:362–379. PMID: 8346839.
Article20. Lee C, Jang MS, Song YK, O S, Moon SY, Kang DB, et al. The effect of magnesium sulfate on postoperative pain in patients undergoing major abdominal surgery under remifentanil-based anesthesia. Korean J Anesthesiol. 2008; 55:286–290.
Article21. Ko SH, Jang YI, Lee JR, Han YJ, Choe H. Effects of preincisional administration of magnesium sulfate on postoperative pain and recovery of pulmonary function in patients undergoing gastrectomy. J Korean Pain Soc. 2000; 13:31–37.22. Gunduz A, Bilir A, Gulec S. Magnesium added to prilocaine prolongs the duration of axillary plexus block. Reg Anesth Pain Med. 2006; 31:233–236. PMID: 16701189.
Article23. Goyal P, Jaiswal R, Hooda S, Goyal R, Lal J. Role of magnesium sulphate for brachial plexus analgesia. Internet J Anesthesiol [serial on the Internet]. 2009. 7. 2009 Jul 15. Avaiable at http://www.ispub.com/journal/the_internet_journal_of_anesthesiology/volume_21_number_1/article/role-of-magnesium-sulphate-for-brachial-plexus-analgesia.html.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effects of Postoperative Brachial Plexus Block Using MgSO4 on the Postoperative Pain after Upper Extremity Surgery
- Continuous Axillary Brachial Plexus Block after Upper Extremity Operation
- Bilateral Interscalene Brachial Plexus Block for Surgery on Both Upper Extremities in a Patient with Unilateral Vocal Cord Paralysis : A case report
- The Effect of Morphine administered with Bupivacaine in Brachial Plexus Block
- The Efficacy of Ultrasound-Guided Brachial Plexus Block in Trauma Patients