Comparison of Diagnostic Utility between Procalcitonin and C-Reactive Protein for the Patients with Blood Culture-Positive Sepsis
- Affiliations
-
- 1Department of Laboratory Medicine, Konkuk University School of Medicine, Seoul, Korea. dearmina@hanmail.net
- 2Department of Laboratory Medicine, Hallym University College of Medicine, Seoul, Korea.
- KMID: 1781606
- DOI: http://doi.org/10.3343/kjlm.2009.29.6.529
Abstract
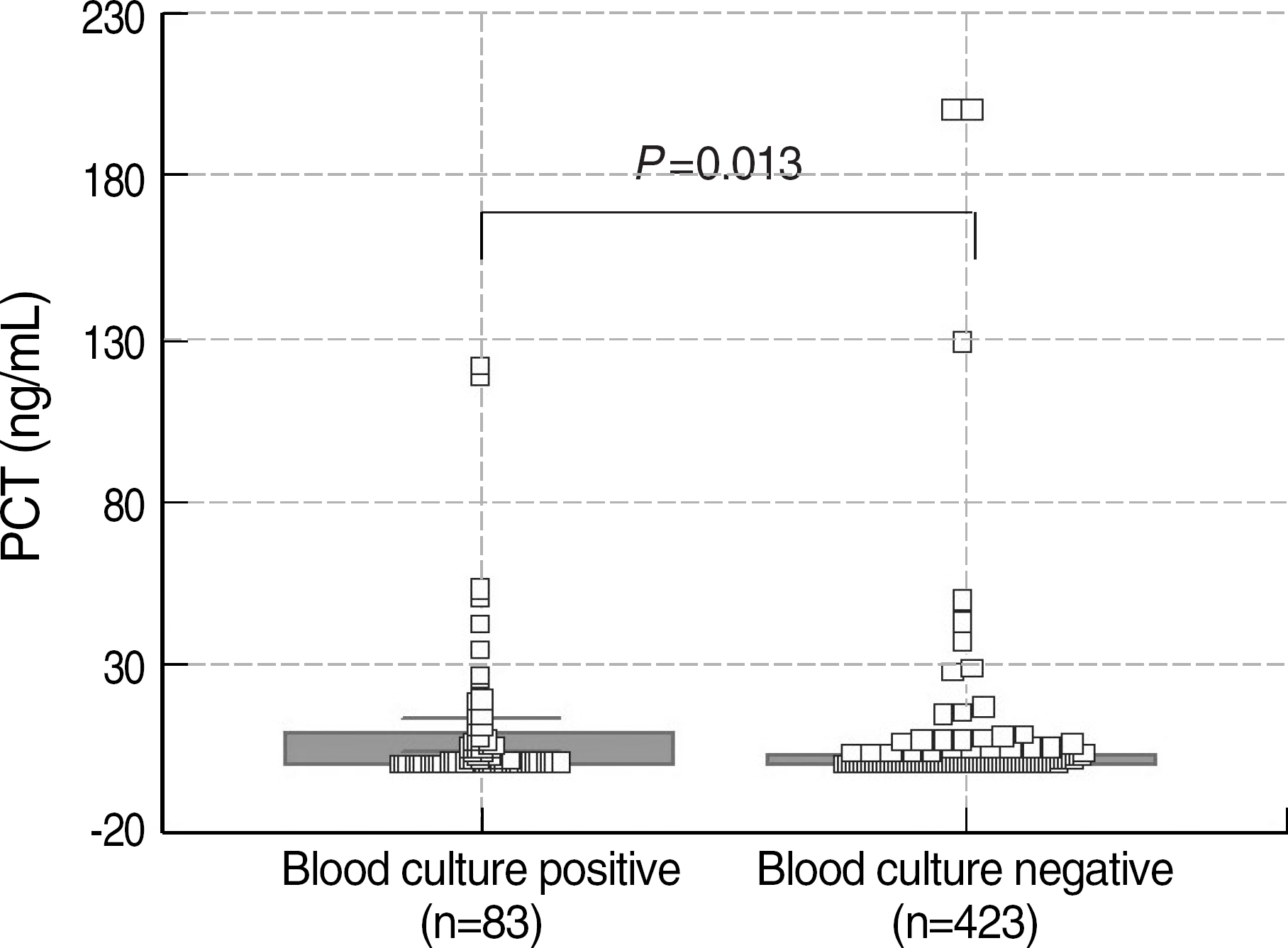
- BACKGROUND
Procalcitonin (PCT) is a relatively new marker for bacterial infections, and its diagnostic utility has been variable across the studies. We investigated the diagnostic utility of PCT for the patients with blood culture-positive sepsis, and compared it with that of C-reactive protein (CRP). METHODS: In 1,270 consecutive blood samples, PCT and CRP were simultaneously measured and results were compared according to the five categories of PCT concentrations (<0.05 ng/mL; 0.05-0.49 ng/mL; 0.5-1.99 ng/mL; 2-9.99 ng/mL; > or =10 ng/mL). In 506 samples, they were further analyzed according to the result of blood culture. PCT and CRP were measured using enzyme-linked fluorescent assay (bioMerieux Co., France) and rate nephelometry (Beckman Coulter Co., USA), respectively. Their diagnostic utilities were compared using ROC curves. RESULTS: The mean concentrations of CRP in five categories of PCT were 15.4 mg/L, 42.1 mg/L, 101.2 mg/L, 125.0 mg/L, 167.1 mg/L, respectively (P<0.0001). Both PCT and CRP showed significant differences between the two positive and negative groups of blood culture (PCT, 8.47 vs 2.44 ng/mL, P=0.0133; CRP, 110.48 vs 59.78 mg/L, P<0.0001). The areas under the ROC curves (95% confidence interval) for PCT and CRP were 0.720 (0.644-0.788) and 0.558 (0.478-0.636), respectively, and showed a significant difference (P=0.005). CONCLUSIONS: The diagnostic utility of PCT is superior to that of CRP for the patients with blood culture-positive sepsis. PCT seems to be reliable for sepsis diagnosis, and may provide useful information for the critically ill patients.
Keyword
MeSH Terms
-
Adolescent
Adult
Aged
Aged, 80 and over
Biological Markers/blood
C-Reactive Protein/*analysis
Calcitonin/*blood
Child
Child, Preschool
Enzyme-Linked Immunosorbent Assay
Humans
Infant
Infant, Newborn
Middle Aged
Nephelometry and Turbidimetry
Protein Precursors/*blood
ROC Curve
Reagent Kits, Diagnostic
Sensitivity and Specificity
Sepsis/*diagnosis
Figure
Cited by 4 articles
-
Utility of Procalcitonin as an Early Diagnostic Marker of Bacteremia in Patients with Acute Fever
Myeong Hee Kim, Gayoung Lim, So Young Kang, Woo-In Lee, Jin-Tae Suh, Hee Joo Lee
Yonsei Med J. 2011;52(2):276-281. doi: 10.3349/ymj.2011.52.2.276.Diagnostic value of procalcitonin and CRP in critically ill patients admitted with suspected sepsis
Jae-Sik Joen, Sung-Mi Ji
J Dent Anesth Pain Med. 2015;15(3):135-140. doi: 10.17245/jdapm.2015.15.3.135.The Value of Serum Procalcitonin Level for Differentiation between Contaminants and Pathogens in Bacteremia
Hei Kyung Jin, Jae Yun Jang, Young Uh, Ohgun Kwon, Kap Jun Yoon, Hyo Youl Kim, Young Keun Kim
Korean J Clin Microbiol. 2011;14(1):7-12. doi: 10.5145/KJCM.2011.14.1.7.Predictive value of C-reactive protein for the diagnosis of meningitis in febrile infants under 3 months of age in the emergency department
Tae Gyoung Lee, Seung Taek Yu, Cheol Hwan So
Yeungnam Univ J Med. 2020;37(2):106-111. doi: 10.12701/yujm.2019.00402.
Reference
-
1.Pfäfflin A., Schleicher E. Inflammation markers in point-of-care testing (POCT). Anal Bioanal Chem. 2009. 393:1473–80.
Article2.American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med. 1992. 20:864–74.3.Levy MM., Fink MP., Marshall JC., Abraham E., Angus D., Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003. 31:1250–6.
Article4.Mitaka C. Clinical laboratory differentiation of infectious versus non-infectious systemic inflammatory response syndrome. Clin Chim Acta. 2005. 351:17–29.
Article5.Meisner M. Pathobiochemistry and clinical use of procalcitonin. Clin Chim Acta. 2002. 323:17–29.
Article6.Becker KL., Snider R., Nylen ES. Procalcitonin assay in systemic inflammation, infection, and sepsis: clinical utility and limitations. Crit Care Med. 2008. 36:941–52.
Article7.Chua AP., Lee KH. Procalcitonin in severe acute respiratory syndrome (SARS). J Infect. 2004. 48:303–6.
Article8.Cone JB. Inflammation. Am J Surg. 2001. 182:558–62.
Article9.Luster AD. Chemokines-chemotactic cytokines that mediate inflammation. N Engl J Med. 1998. 338:436–45.10.Simon L., Gauvin F., Amre DK., Saint-Louis P., Lacroix J. Serum pro-calcitonin and C-reactive protein levels as markers of bacterial infection: a systematic review and meta-analysis. Clin Infect Dis. 2004. 39:206–17.
Article11.Whicher J., Bienvenu J., Monneret G. Procalcitonin as an acute phase marker. Ann Clin Biochem. 2001. 38:483–93.
Article12.Nijsten MW., Olinga P., The TH., de Vries EG., Koops HS., Groothuis GM, et al. Procalcitonin behaves as a fast responding acute phase protein in vivo and in vitro. Crit Care Med. 2000. 28:458–61.
Article13.Assicot M., Gendrel D., Carsin H., Raymond J., Guilbaud J., Bohuon C. High serum procalcitonin concentrations in patients with sepsis and infection. Lancet. 1993. 341:515–8.
Article14.Brunkhorst FM., Al-Nawas B., Krummenauer F., Forycki ZF., Shah PM. Procalcitonin, C-reactive protein and APACHE II score for risk evaluation in patients with severe pneumonia. Clin Microbiol Infect. 2002. 8:93–100.
Article15.Oberhoffer M., Vogelsang H., Russwurm S., Hartung T., Reinhart K. Outcome prediction by traditional and new markers of inflammation in patients with sepsis. Clin Chem Lab Med. 1999. 37:363–8.
Article16.Rau BM., Frigerio I., Büchler MW., Wegscheider K., Bassi C., Puolakkainen PA, et al. Evaluation of procalcitonin for predicting septic multiorgan failure and overall prognosis in secondary peritonitis: a prospective, international multicenter study. Arch Surg. 2007. 142:134–42.17.Rau B., Krüger CM., Schilling MK. Procalcitonin: improved biochemical severity stratification and postoperative monitoring in severe abdominal inflammation and sepsis. Langenbecks Arch Surg. 2004. 389:134–44.
Article18.Liaudat S., Dayer E., Praz G., Bille J., Troillet N. Usefulness of procalcitonin serum level for the diagnosis of bacteremia. Eur J Clin Microbiol Infect Dis. 2001. 20:524–7.
Article19.Whang KT., Steinwald PM., White JC., Nylen ES., Snider RH., Simon GL, et al. Serum calcitonin precursors in sepsis and systemic inflammation. J Clin Endocrinol Metab. 1998. 83:3296–301.
Article20.Uzzan B., Cohen R., Nicolas P., Cucherat M., Perret GY. Procalcitonin as a diagnostic test for sepsis in critically ill adults and after surgery or trauma: a systematic review and meta-analysis. Crit Care Med. 2006. 34:1996–2003.
Article21.Boussekey N., Leroy O., Georges H., Devos P., d'Escrivan T., Guery B. Diagnostic and prognostic values of admission procalcitonin levels in community-acquired pneumonia in an intensive care unit. Infection. 2005. 33:257–63.
Article22.Thayyil S., Shenoy M., Hamaluba M., Gupta A., Frater J., Verber IG. Is procalcitonin useful in early diagnosis of serious bacterial infections in children? Acta Paediatr. 2005. 94:155–8.
Article23.Harbarth S., Holeckova K., Froidevaux C., Pittet D., Ricou B., Grau GE, et al. Diagnostic value of procalcitonin, interleukin-6 and interleukin-8 in critically ill patients admitted with suspected sepsis. Am J Respir Crit Care Med. 2001. 164:396–402.
Article24.Müller B., Becker KL., Schächinger H., Rickenbacher PR., Huber PR., Zimmerli W, et al. Calcitonin precursors are reliable markers of sepsis in a medical intensive care unit. Crit Care Med. 2000. 28:977–83.
Article25.Povoa P., Almeida E., Moreira P., Fernandes A., Mealha R., Aragao A, et al. C-reactive protein as an indicator of sepsis. Intensive Care Med. 1998. 24:1052–6.26.Aikawa N., Fujishima S., Endo S., Sekine I., Kogawa K., Yamamoto Y, et al. Multicenter prospective study of procalcitonin as an indicator of sepsis. J Infect Chemother. 2005. 11:152–9.
Article27.Endo S., Aikawa N., Fujishima S., Sekine I., Kogawa K., Yamamoto Y, et al. Usefulness of procalcitonin serum level for the discrimination of severe sepsis from sepsis: a multicenter prospective study. J Infect Chemother. 2008. 14:244–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Diagnostic Utility between Procalcitonin and C-Reactive Protein for the Patients with Blood Culture-Positive Sepsis
- Diagnostic value of procalcitonin and CRP in critically ill patients admitted with suspected sepsis
- Clinical utility of procalcitonin in severe odontogenic maxillofacial infection
- Clinical Use of Procalcitonin in the Diagnosis of Sepsis: Evaluation of PCT–qSOFA
- Delta Neutrophil Index as an Early Marker of Sepsis in Burn Patients