J Korean Ophthalmol Soc.
2011 Sep;52(9):1039-1047.
Two-Year Results of Intravitreal Bevacizumab Injection in Retinal Vein Occlusion
- Affiliations
-
- 1Department of Ophthalmology, Kyung Hee University School of Medicine, Seoul, Korea. syyu@khu.ac.kr
- 2Department of Ophthalmology, Inje University College of Medicine, Seoul, Korea.
Abstract
- PURPOSE
The authors evaluated the 2-year clinical results of intravitreal bevacizumab injection in retinal vein occlusion (RVO).
METHODS
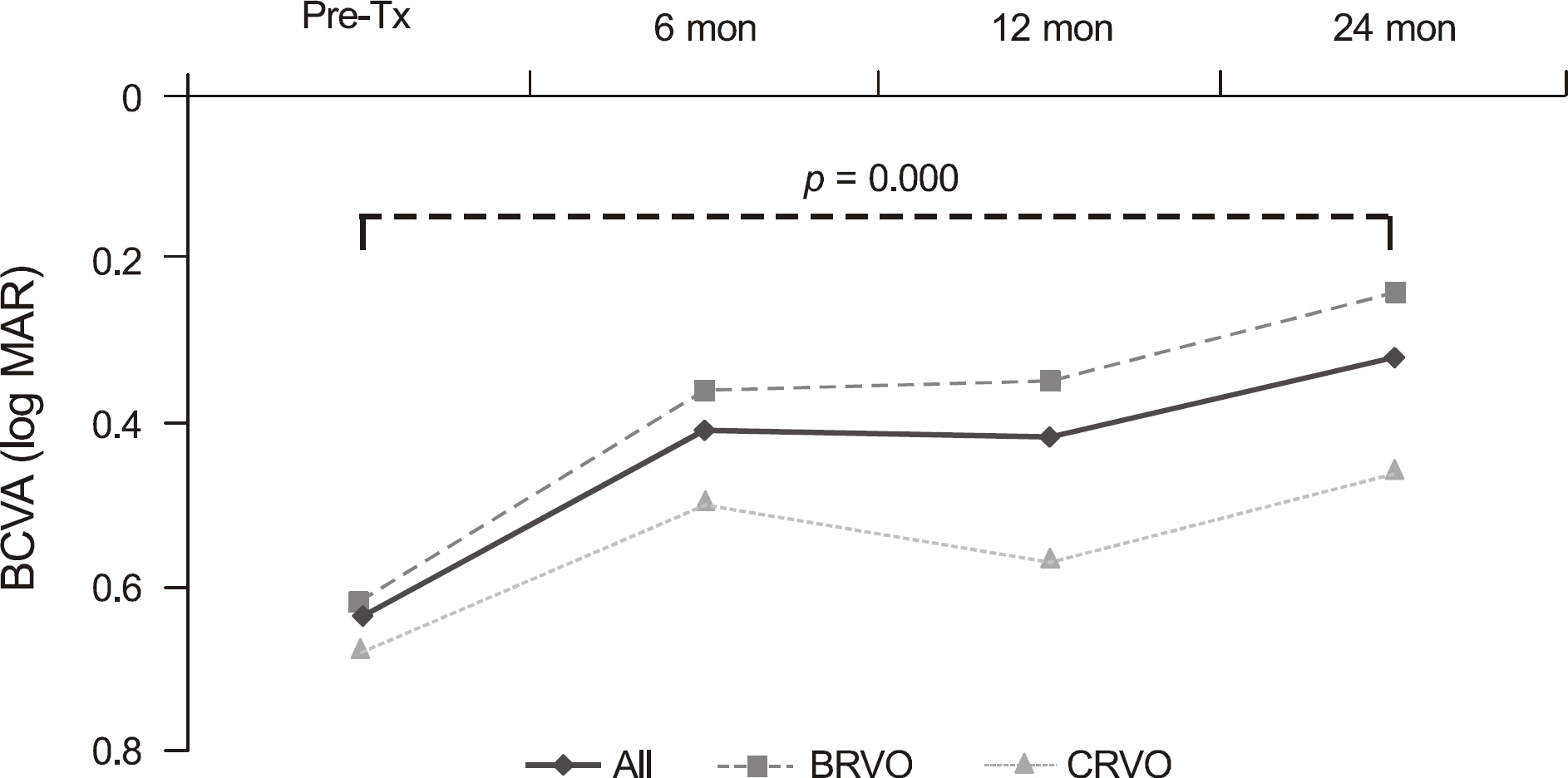
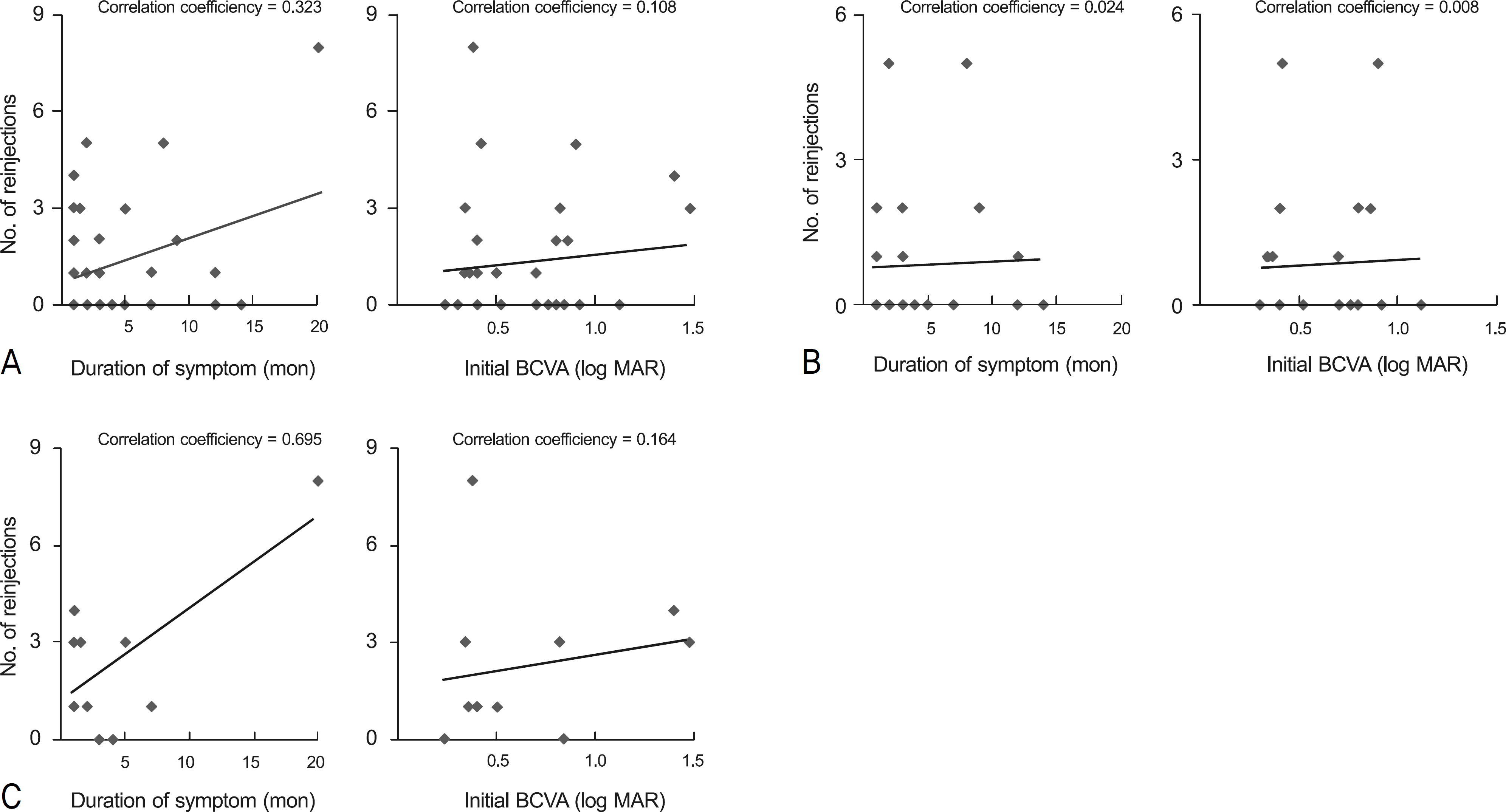
Thirty-two eyes of 32 patients treated with an intravitreal bevacizumab injection of 1.25 mg (0.05 ml) for RVO (branch RVO: 22 eyes, central RVO: 10 eyes), repeated 3 times at a 6-week interval and were available for a follow-up period of at least 2 years were retrospectively reviewed. Best-corrected visual acuity (BCVA) before treatment and 6, 12, and 24 months after 3 serial injections, was recorded. The optical coherence tomography (OCT) results were analyzed to identify prognostic factors for recurrent macular edema that needed reinjection.
RESULTS
Two years after the treatment, mean BCVA was significantly improved (p = 0.000). Out of 32 eyes, 16 (branch RVO: 8 eyes; central RVO: 8 eyes) needed reinjection because of recurrent macular edema. In central RVO, a significantly high reinjection rate was shown in serous retinal detachment (SRD) compared with cystoid macular edema (CME) as identified in OCT findings (p = 0.049). Additionally, in branch RVO, a high reinjection rate was shown in SRD, although statistically not significant (p = 0.375).
CONCLUSIONS
In patients with RVO, a significant visual improvement was maintained for at least 2 years after intravitreal bevacizumab injection. Based on OCT results, SRD showed a high reinjection rate compared with CME in CRVO.
MeSH Terms
Figure
Reference
-
References
1. Mitchell P, Smith W, Chang A. Prevalence and associations of retinal vein occlusion. The Blue Mountains Eye Study. Arch Ophthalmol. 1996; 114:1243–7.2. Ryan SJ. Retina. Dick SB, Jampol LM, Haller JA, editors. Macular Edema. 3rd ed.St. Louis: The C.V. Mosby Co;2001. 2:chap.p. 57.3. Argon laser photocoagulation for macular edema in branch vein occlusion. The Branch Vein Occlusion Study Group. Am J Ophthalmol. 1984; 98:271–82.4. Evaluation of grid pattern photocoagulation for macular edema in central vein occlusion. The Central Vein Occlusion Study Group M report. Ophthalmology. 1995; 102:1425–33.5. Jonas JB, Hayler JK, Panda-Jonas S. Intravitreal injection of crystalline cortisone as adjunctive treatment of proliferative vitreoretinopathy. Br J Ophthalmol. 2000; 84:1064–7.
Article6. Shin JH, Lee SW, Kim DK, et al. Intravitreal injection of triamcinolone acetonide for macular edema: long-term safety and efficacy after two years. J Korean Ophthalmol Soc. 2007; 48:1670–4.7. Martidis A, Duker JS, Greenberg PB, et al. Intravitreal triamcinolone for refractory diabetic macular edema. Ophthalmology. 2002; 109:920–7.
Article8. Greenberg PB, Martidis A, Rogers AH, et al. Intravitreal triamcinolone acetonide for macular oedema due to central retinal vein occlusion. Br J Ophthalmol. 2002; 86:247–8.
Article9. Tolentino MJ, Miller JW, Gragoudas ES, et al. Intravitreous injections of vascular endothelial growth factor produce retinal ischemia and microangiopathy in an adult primate. Ophthalmology. 1996; 103:1820–8.
Article10. Noma H, Funatsu H, Yamasaki M, et al. Pathogenesis of macular edema with branch retinal vein occlusion and intraocular levels of vascular endothelial growth factor and interleukin-6. Am J Ophthalmol. 2005; 140:256–61.
Article11. Rosenfeld PJ, Moshfeghi AA, Puliafito CA. Optical coherence tomography findings after an intravitreal injection of bevacizumab (avastin) for neovascular age-related macular degeneration. Ophthalmic Surg Lasers Imaging. 2005; 36:331–5.
Article12. Wu L, Arevalo JF, Roca JA, et al. Comparison of two doses of intravitreal bevacizumab (Avastin) for treatment of macular edema secondary to branch retinal vein occlusion: results from the Pan-American Collaborative Retina Study Group at 6 months of follow-up. Retina. 2008; 28:212–9.13. Lee SW, Kim MS, Kim ES, et al. Long-term results of intravitreal bevacizumab injection for macular edema: retinal vein obstruction and diabetic retinopathy. J Korean Ophthalmol Soc. 2009; 50:211–8.
Article14. Prager F, Michels S, Kriechbaum K, et al. Intravitreal bevacizumab (Avastin®) for macular oedema secondary to retinal vein occlusion: 12-month results of a prospective clinical trial. Br J Ophthalmol. 2009; 93:452–6.15. Gutierrez JC, Barquet LA, Caminal JM, et al. Intravitreal bevacizumab (Avastin) in the treatment of macular edema secondary to retinal vein occlusion. Clin Ophthalmol. 2008; 2:787–91.16. Hoeh AE, Ach T, Schaal KB, et al. Long-term follow-up of OCT-guided bevacizumab treatment of macular edema due to retinal vein occlusion. Graefes Arch Clin Exp ophthalmol. 2009; 247:1635–41.
Article17. Kondo M, Kondo N, Ito Y, et al. Intravitreal injection of bevacizumab for macular edema secondary to branch retinal vein occlusion: results after 12 months and multiple regression analysis. Retina. 2009; 29:1242–8.18. Stahl A, Struebin I, Hansen LL, et al. Bevacizumab in central retinal vein occlusion: a retrospective analysis after 2 years of treatment. Eur J Ophthalmol. 2010; 20:180–5.
Article19. Gregori NZ, Rattan GH, Rosenfeld PJ, et al. Safety and efficacy of intravitreal bevacizumab(Avastin) for the management of branch and hemiretinal vein occlusion. Retina. 2009; 29:913–25.20. Gregori NZ, Gaitan J, Rosenfeld PJ, et al. Long-term safety and efficacy of intravitreal bevacizumab(Avastin) for the management of central retinal vein occlusion. Retina. 2008; 28:1325–37.21. Hung KH, Lee SM, Lee SY, et al. Intravitreal bevacizumab (Avastin) in the treatment of macular edema associated with perfused retinal vein occlusion. J Ocul Pharmacol Ther. 2010; 26:85–90.
Article22. Beutel J, Ziemssen F, Luke M, et al. Intravitreal bevacizumab treatment of macular edema in central retinal vein occlusion: one-year results. Int Ophthalmol. 2010; 30:15–22.
Article23. Chung EJ, Hong YT, Lee SC, et al. Prognostic factors for visual outcome after intravitreal bevacizumab for macular edema due to branch retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2008; 246:1241–7.
Article24. Ach T, Hoeh AE, Schaal KB, et al. Predictive factors for changes in macular edema in intravitreal bevacizumab therapy of retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2010; 248:155–9.
Article25. Otani T, Kishi S, Maruyama Y. Patterns of diabetic macular edema with optical coherence tomography. Am J Ophthalmol. 1999; 127:688–93.
Article26. Ferrara N. Vascular endothelial growth factor: molecular and biological aspects. Curr Top Microbiol Immunol. 1999; 237:1–30.
Article27. Aiello LP, Northrup JM, Keyt BA, et al. Hypoxic regulation of vascular endothelial growth factor in retinal cells. Arch ophthalmol. 1995; 113:1538–44.
Article28. Duff IF, Falls HF, Linman JW. Anticoagulant therapy in occlusive vascular disease of the retina. Ama Arch Ophthalmol. 1951; 46:601–17.
Article29. Michels RG, Gass JD. The natural course of retinal branch vein obstruction. Trans Am Acad Ophthalmol Otolaryngol. 1974; 78:166–77.
Article30. Zhang Y, Fortune B, Atchaneeyasakul LO, et al. Natural history and histology in a rat model of laser-induced photothrombotic retinal vein occlusion. Curr Eye Res. 2008; 33:365–76.
Article31. Kim SH, Park JM. Comparison of intravitreal triamcinolone versus bevacizumab in bilateral diabetic macular edema by optical coherence tomography (OCT) patterns. J Korean Ophthalmol Soc. 2010; 51:210–9.
Article32. Jalkh AE, Trempe CL. Macular edema in branch retinal vein occlusion: types and treatment. Ophthalmic Surg. 1989; 20:26–32.
Article33. Rehak J. Retinal vein occlusion. I. Pathogenesis of circulatory changes. Cesk Oftalmol. 1993; 49:145–7.34. Finkelstein D. Ischemic macular edema. Recognition and favorable natural history in branch vein occlusion. Arch Ophthalmol. 1992; 110:1427–34.
Article35. Yanoff M, Fine BS, Brucker AJ, et al. Pathology of human cystoid macular edema. Surv Ophthalmol. 1984; 28:505–11.
Article36. Schatz H, Yannuzzi L, Stransky TJ. Retinal detachment secondary to branch vein occlusion: part 2. Ann Ophthalmol. 1976; 8:1461–71.37. Lee SW, Kim HK, Kim SY. Patterns of macular edema in patients with branch retinal vein occlusion on optical coherence tomography. J Korean Ophthalmol Soc. 2005; 46:969–75.38. Song YB, Park SP. Short-term effects of intravitreal bevacizumab injection and macular edema patterns in branch retinal vein occlusion. J Korean Ophthalmol Soc. 2010; 51:379–85.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Retinal Hemorrhage Following a Dexamethasone Intravitreal Implant
- Comparison of Bevacizumab and Combined Low-dose Bevacizumab and Triamcinolone in Central Retinal Vein Occlusion
- Combined Low Dose Bevacizumab-triamcinolone versus Bevacizumab Single Intravitreal Injection for Branch Retinal Vein Occlusion
- Macular Vessel Density Analysis Using Optical Coherence Tomography Angiography before and after Intravitreal Bevacizumab Injection in Branch Retinal Vein Occlusion
- The Efficacy of Intravitreal Bevacizumab in the Treatment of Macular Edema