J Korean Ophthalmol Soc.
2011 Mar;52(3):299-307. 10.3341/jkos.2011.52.3.299.
Macular Thickness Changes with Age and Gender in Emmetropia Using Spectral Domain Optical Coherence Tomography
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine, Soonchunhyang University, Seoul, Korea. wismile@unitel.co.kr
- KMID: 2214294
- DOI: http://doi.org/10.3341/jkos.2011.52.3.299
Abstract
- PURPOSE
To evaluate the changes in macular thickness with regard to age and gender in normal subjects with emmetropia using spectral domain optical coherence tomography.
METHODS
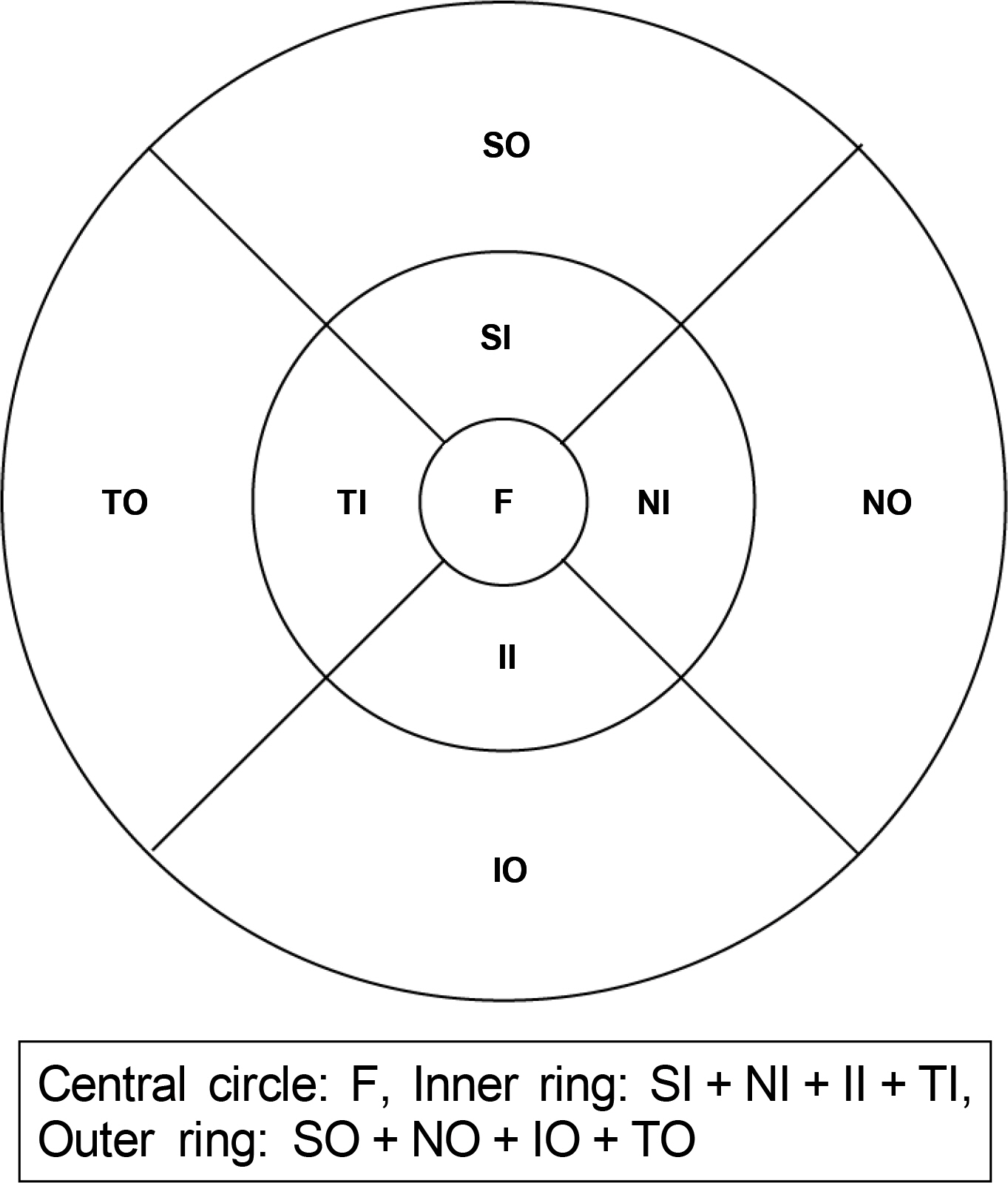
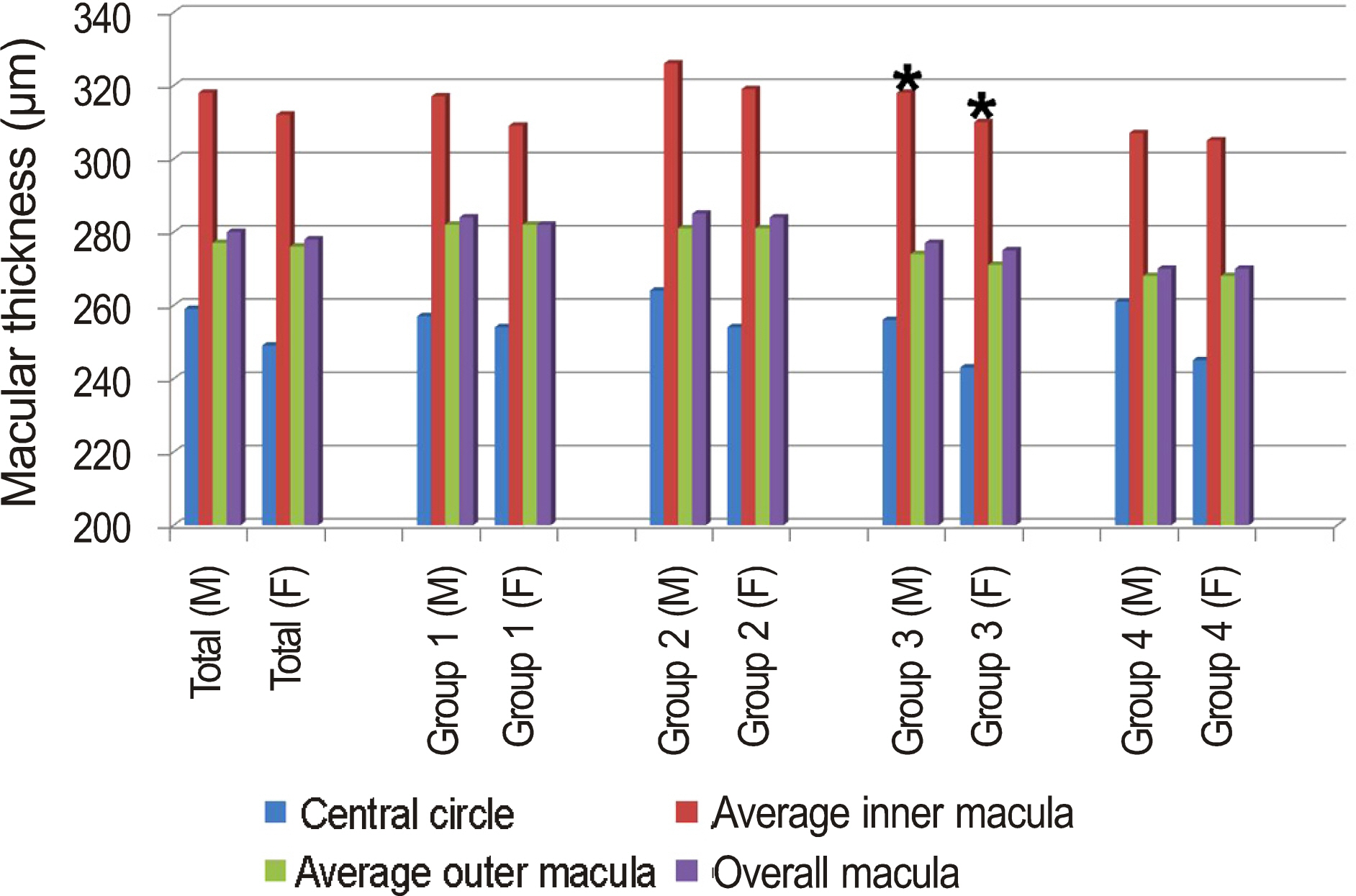
The present study consisted of 90 healthy subjects (162 eyes) with no ophthalmic evidence of retinopathy and who had emmetropic eyes. The data from macular measurements using spectral domain optical coherence tomography was analyzed according to the groups divided by age (Group 1: 0 to 19 years of age, Group 2: 20 to 39 years of age, Group 3: 40 to 59 years of age, Group 4: 60 to 80 years of age) and gender.
RESULTS
Macular thickness of the central circle was 253.40 +/- 23.03 microm in all subjects. There was no significant change with age (p > 0.05). However, the measurements at the inner (3 mm) and outer circle (6 mm) showed a reduction of macular thickness with age (p < 0.05). The macular thickness at the central and inner circle was significantly lower in the female subjects (p < 0.05). In group 3 and 4, macular thickness at the central circle in males was greater than in females. In group 3, the average inner macular thickness in males was significantly greater than in females (p < 0.05).
CONCLUSIONS
In normal subjects with emmetropia, there are statistically significant differences in macular thickness between subjects of different age and gender. The results from the present study can be expected to provide a reference value for evaluating macular disease.
Figure
Cited by 3 articles
-
Foveal Shape According to Age and Gender Using Spectral Domain Optical Coherence Tomography
Min Byung Chae, Jae Suk Kim
J Korean Ophthalmol Soc. 2014;55(10):1504-1510. doi: 10.3341/jkos.2014.55.10.1504.A Study of Foveal Shape in Emmetropia and Myopia Using Spectral Domain Optical Coherence Tomography
Min Seok Kim, Jae Suk Kim, Jin Choi, Jung Hoon Kim, Won Hyuk Oh
J Korean Ophthalmol Soc. 2014;55(6):833-839. doi: 10.3341/jkos.2014.55.6.833.Analysis of Macular Layer Thickness Measured Using Spectral Domain Optical Coherence Tomography in Korean Subjects
Chung Hwan Kim, Sun Young Jin, Young Hoon Lee, Young Suk Chang
J Korean Ophthalmol Soc. 2016;57(2):264-275. doi: 10.3341/jkos.2016.57.2.264.
Reference
-
References
1. Puliafito CA, Hee MR, Lin CP, et al. Imaging of macular diseases with optical coherence tomography. Ophthalmology. 1995; 102:217–29.
Article2. Muscat S, Parks S, Kemp E, Keating D. Repeatability and reproducibility of macular thickness measurements with the Humphrey OCT system. Invest Ophthalmol Vis Sci. 2002; 43:490–5.3. Chen TC, Cense B, Pierce MC, et al. Spectral domain optical coherence tomography: ultra-high speed, ultra-high resolution ophthalmic imaging. Arch Ophthalmol. 2005; 123:1715–20.4. Yi K, Chen TC, de Boer JF. Spectral domain optical coherence tomography. Tech Ophthalmol. 2006; 4:170–4.
Article5. Ahlers C, Michels S, Beckendorf A, et al. Three-dimensional imaging of pigment epithelial detachment in age-related macular degeneration using optical coherence tomography, retinal thickness analysis and topographic angiography. Graefes Arch Clin Exp Ophthalmol. 2006; 244:1233–9.
Article6. Kim CS, Kim SY, Park YH, Lee YC. Change in ocular dimensions with age in patients with emmetropia. J Korean Ophthalmol Soc. 2008; 49:425–32.
Article7. Panda-Jonas S, Jonas JB, Jakobczyk-Zmija M. Retinal photoreceptor density decreases with age. Ophthalmology. 1995; 102:1853–9.
Article8. Gao H, Hollyfield JG. Aging of the human retina. Differential loss of neurons and retinal pigment epithelial cells. Invest Ophthalmol Vis Sci. 1992; 33:1–17.9. Repka MX, Quigley HA. The effect of age on normal human optic nerve fiber number and diameter. Ophthalmology. 1989; 96:26–32.10. Balazsi AG, Rootman J, Drance SM, et al. The effect of age on the nerve fiber population of the human optic nerve. Am J Ophthalmol. 1984; 97:760–6.
Article11. Eriksson U, Alm A. Macular thickness decreases with age in normal eyes: a study on the macular thickness map protocol in the Stratus OCT. Br J Ophthalmol. 2009; 93:1448–52.
Article12. Göbel W, Hartmann F, Haigis W. Determination of retinal thickness in relation to the age and axial length using optical coherence tomography. Ophthalmologe. 2001; 98:157–62.13. Zou H, Zhang X, Xu X, Yu S. Quantitative in vivo retinal thickness measurement in chinese healthy subjects with retinal thickness analyzer. Invest Ophthalmol Vis Sci. 2006; 47:341–7.
Article14. Kanai K, Abe T, Murayama K, Yoneya S. Retinal thickness and changes with age. Nippon Ganka Gakkai Zasshi. 2002; 106:162–5.
Article15. Alamouti B, Funk J. Retinal thickness decreases with age: an OCT study. Br J Ophthalmol. 2003; 87:899–901.
Article16. Neuville JM, Bronson-Castain K, Bearse MA Jr, et al. OCT reveals regional differences in macular thickness with age. Optom Vis Sci. 2009; 86:E810–6.
Article17. Duan XR, Liang YB, Friedman DS, et al. Normal macular thickness measurements using optical coherence tomography in healthy eyes of adult Chinese persons: the Handan Eye Study. Ophthalmology. 2010; 117:1585–94.
Article18. Wong AC, Chan CW, Hui SP. Relationship of gender, body mass index, and axial length with central retinal thickness using optical coherence tomography. Eye. 2005; 19:292–7.
Article19. Kleinstein RN, Jones LA, Hullett S, et al. Refractive error and eth-nicity in children. Arch Ophthalmol. 2003; 121:1141–7.
Article20. Nussenblatt RB, Kaufman SC, Palestine AG, et al. Macular thick-ening and visual acuity. Measurement in patients with cystoid macular edema. Ophthalmology. 1987; 94:1134–9.21. Kang JH, Kim SA, Song WG, Yoon HS. Macular thickness changes with age in normal subjects measured by optical coherence tomography. J Korean Ophthalmol Soc. 2004; 45:592–8.22. Song WK, Lee SC, Lee ES, et al. Macular thickness variations with sex, age, and axial length in healthy subjects: a spectral do-main-optical coherence tomography study. Invest Ophthalmol Vis Sci. 2010; 51:3913–8.
Article23. Sung KR, Wollstein G, Bilonick RA, et al. Effects of age on optical coherence tomography measurements of healthy retinal nerve fiber layer, macula, and optic nerve head. Ophthalmology. 2009; 116:1119–24.
Article24. Wakitani Y, Sasoh M, Sugimoto M, et al. Macular thickness measurements in healthy subjects with different axial lengths using optical coherence tomography. Retina. 2003; 23:177–82.
Article25. Huynh SC, Wang XY, Rochtchina E, Mitchell P. Distribution of macular thickness by optical coherence tomography: findings from a population-based study of 6-year-old children. Invest Ophthalmol Vis Sci. 2006; 47:2351–7.
Article26. Kang MS, Kyung SE, Chang MH. Mean macular volume in normal Korean eyes measured by spectral-domain optical coherence tomography. J Korean Ophthalmol Soc. 2010; 51:1077–83.
Article27. Best PJ, Berger PB, Miller VM, Lerman A. The effect of estrogen replacement therapy on plasma nitric oxide and endothelin-1 levels in postmenopausal women. Ann Intern Med. 1998; 128:285–8.
Article28. Moon HJ, Um MJ, Jung H. Changes in superoxide dismutase activities in the erythrocytes of women; correlation of age and serum estrogens concentration. J Korean Soc Menopause. 2004; 10:21–6.29. Liang FQ, Godley BF. Oxidative stress-induced mitochondrial DNA damage in human retinal pigment epithelial cells: a possible mechanism for RPE aging and age-related macular degeneration. Exp Eye Res. 2003; 76:397–403.
Article30. Yu X, Tang Y, Li F, et al. Protection against hydrogen peroxide-induced cell death in cultured human retinal pigment epithelial cells by 17beta-estradiol: a differential gene expression profile. Mech Ageing Dev. 2005; 126:1135–45.31. Lattanzio R, Brancato R, Pierro L, et al. Macular thickness measured by optical coherence tomography (OCT) in diabetic patients. Eur J Ophthalmol. 2002; 12:482–7.
Article32. Goebel W, Kretzchmar-Gross T. Retinal thickness in diabetic retinopathy: a study using optical coherence tomography (OCT). Retina. 2002; 22:759–67.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Macular Thickness Changes with Age and Gender in Emmetropia Using Spectral Domain Optical Coherence Tomography
- Analysis of Factors Associated with Variability in Measures Obtained by Spectral Domain Optical Coherence Tomography
- A Study of Foveal Shape in Emmetropia and Myopia Using Spectral Domain Optical Coherence Tomography
- Repeatability of Spectral Domain OCT (3D-OCT 1000) in Normal Subjects and Various Macular Diseases
- Analysis of Macular Layer Thickness Measured Using Spectral Domain Optical Coherence Tomography in Korean Subjects