J Korean Ophthalmol Soc.
2009 Dec;50(12):1840-1846. 10.3341/jkos.2009.50.12.1840.
Quantitative Analysis of Retinal Nerve Fiber Layer Thickness Profile in Myopic Eyes
- Affiliations
-
- 1Department of Ophthalmology, Hallym University College of Medicine, Kang Dong Sacred Heart Hospital, Seoul, Korea. yaromil@gmail.com
- KMID: 2212996
- DOI: http://doi.org/10.3341/jkos.2009.50.12.1840
Abstract
- PURPOSE
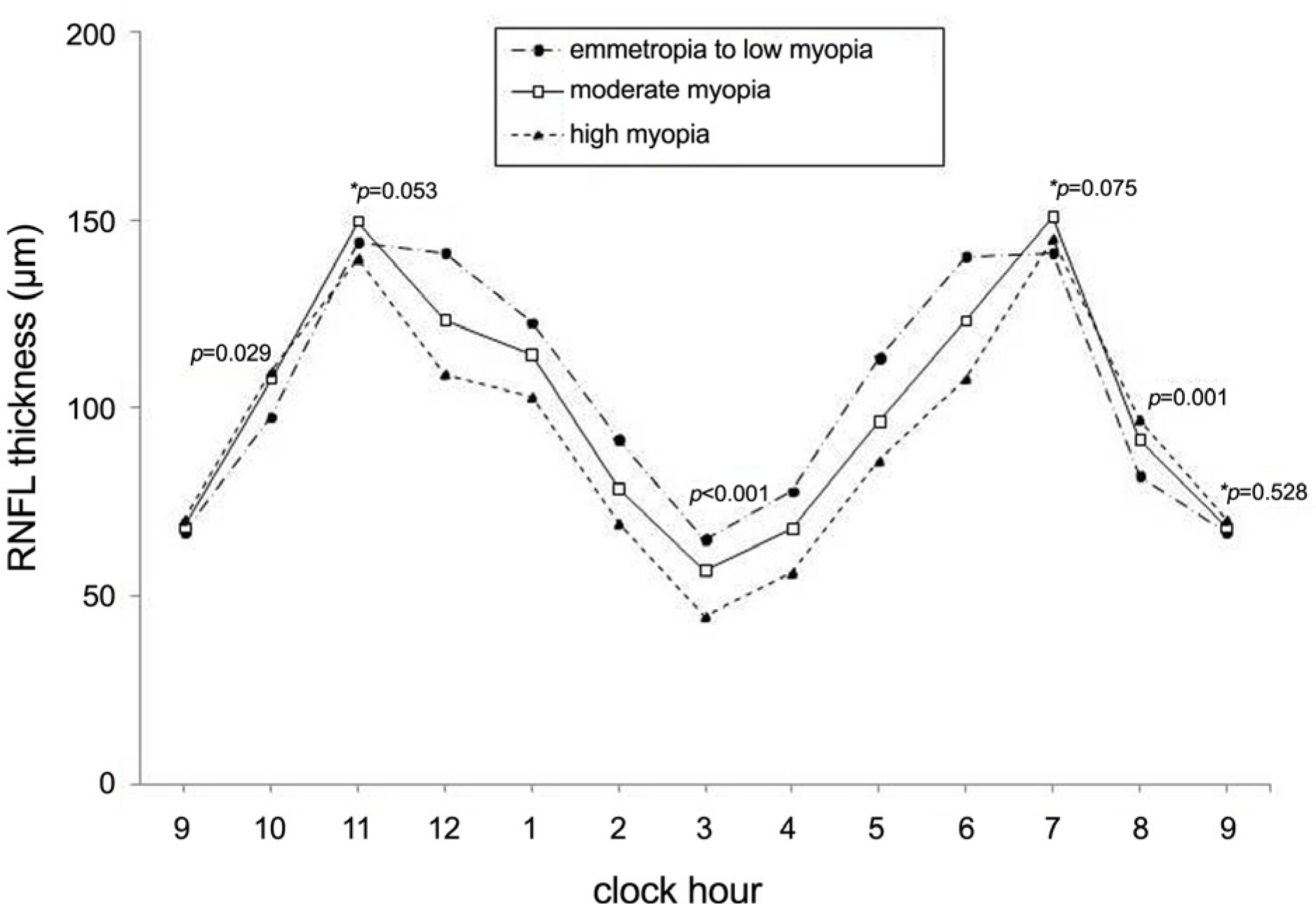
To investigate peripapillary retinal nerve fiber layer (RNFL) thickness profiles associated with myopia.
METHODS
One hundred and twenty-seven normal eyes of 67 Korean adults were divided into three groups by spherical equivalent. All subjects were tested with fast RNFL scans of Stratus optical coherence tomography. The angular locations of superior and inferior maximal thickness points in relationship to a reference line drawn horizontally though the center of the scan circle were calculated from the raw data of scanned images (angle alpha, angle beta). Differences of angle alpha and angle beta were compared among the three groups.
RESULTS
Angle alpha and angle beta were significantly different in three groups (ANOVA, p<0.001, respectively). Angle alpha and angle beta were also significantly different among the three groups for excluded eyes with tilted discs.
CONCLUSIONS
The points of superior and inferior maximal peripapillary RNFL thickness were significantly different in three groups divided by spherical equivalent. As myopia becomes more severe, superior and inferior maximal peripapillary RNFL thickness points are located closer to the fovea.
Figure
Cited by 1 articles
-
Changes of Peripapillary Retinal Nerve Fiber Layer Thickness Profile According to Aging in Myopic Eyes
Eun Jin Bae, Young Cheol Yoo
J Korean Ophthalmol Soc. 2013;54(7):1066-1073. doi: 10.3341/jkos.2013.54.7.1066.
Reference
-
References
1. Katz J, Tielsch JM, Sommer A. Prevalence and risk factors for refractive errors in an adult inner city population. Invest Ophthalmol Vis Sci. 1997; 38:334–40.2. Wang Q, Klein BE, Klein R, Moss SE. Refractive status in the Beaver Dam Eye Study. Invest Ophthalmol Vis Sci. 1994; 35:4344–7.3. Lin LL, Shih YF, Hsiao CK, et al. Epidemiologic study of the prevalence and severity of myopia among schoolchildren in Taiwan in 2000. J Formos Med Assoc. 2001; 100:684–91.4. Wong TY, Foster PJ, Hee J, et al. Prevalence and risk factors for refractive errors in adult Chinese in Singapore. Invest Ophthalmol Vis Sci. 2000; 41:2486–94.5. Au Eong KG, Tay TH, Lim MK. Race, culture and Myopia in 110,236 young Singaporean males. Singapore Med J. 1993; 34:29–32.6. Tay MT, Au Eong KG, Ng CY, Lim MK. Myopia and educational attainment in 421,116 young Singaporean males. Ann Acad Med Singapore. 1992; 21:785–91.7. Kang SH, Kim PS, Choi DG. Prevalence of myopia in 19-year-old Korean males: The relationship between the prevalence and education or urbanization. J Korean Ophthalmol Soc. 2004; 45:2082–7.8. Podos SM, Becker B, Morton WR. High myopia and primary open-angle glaucoma. Am J Ophthalmol. 1966; 62:1038–43.
Article9. Daubs JG, Crick RP. Effect of refractive error on the risk of ocular hypertension and open angle glaucoma. Trans Ophthalmol Soc U K. 1981; 101:121–6.10. Phelps CD. Effect of myopia on prognosis in treated primary open-angle glaucoma. Am J Ophthalmol. 1982; 93:622–8.
Article11. Perkins ES, Phelps CD. Open angle glaucoma, ocular hypertension, low-tension glaucoma, and refraction. Arch Ophthalmol. 1982; 100:1464–7.
Article12. Wilson MR, Hertzmark E, Walker AM, et al. A case-control study of risk factors in open angle glaucoma. Arch Ophthalmol. 1987; 105:1066–71.
Article13. Mitchell P, Hourihan F, Sandbach J, Wang JJ. The relationship between glaucoma and myopia: The Blue Mountains Eye Study. Ophthalmology. 1999; 106:2010–5.14. Quigley HA, Addicks EM, Green WR, Maumenee AE. Optic nerve damage in human glaucoma. II. The site of injury and susceptibility to damage. Arch Ophthalmol. 1981; 99:635–49.15. Leung CK, Chan WM, Yung WH, et al. Comparison of macular and peripapillary measurements for the detection of glaucoma: an optical coherence tomography study. Ophthalmology. 2005; 112:391–400.16. Hoffmann EM, Medeiros FA, Sample PA, et al. Relationship between patterns of visual field loss and retinal nerve fiber layer thickness measurements. Am J Ophthalmol. 2006; 141:463–71.
Article17. Medeiros FA, Zangwill LM, Bowd C, Weinreb RN. Comparison of the GDx VCC scanning laser polarimeter, HRT II confocal scanning laser ophthalmoscope, and stratus OCT optical coherence tomograph for the detection of glaucoma. Arch Ophthalmol. 2004; 122:827–37.18. Vernon SA, Rotchford AP, Negi A, et al. Peripapillary retinal nerve fibre layer thickness in highly myopic Caucasians as measured by Stratus optical coherence tomography. Br J Ophthalmol. 2008; 92:1076–80.
Article19. Leung CK, Mohamed S, Leung KS, et al. Retinal nerve fiber layer measurements in myopia: An optical coherence tomography study. Invest Ophthalmol Vis Sci. 2006; 47:5171–6.
Article20. Kanamori A, Nakamura M, Escano MF, et al. Evaluation of the glaucomatous damage on retinal nerve fiber layer thickness measured by optical coherence tomography. Am J Ophthalmol. 2003; 135:513–20.
Article21. Caprioli J. The contour of the juxtapapillary nerve fiber layer in glaucoma. Ophthalmology. 1990; 97:358–65.
Article22. Leung CK, Chan WM, Yung WH, et al. Comparison of macular and peripapillary measurements for the detection of glaucoma: an optical coherence tomography study. Ophthalmology. 2005; 112:391–400.23. Sommer A, Miller NR, Pollack I, et al. The nerve fiber layer in the diagnosis of glaucoma. Arch Ophthalmol. 1977; 95:2149–56.
Article24. Tay E, Seah SK, Chan SP, et al. Optic disk ovality as an index of tilt and its relationship to myopia and perimetry. Am J Ophthalmol. 2005; 139:247–52.
Article25. Choi SW, Lee SJ. Thickness changes in the fovea and peripapillary retinal nerve fiber layer depend on the degree of myopia. Korean J Ophthalmol. 2006; 20:215–9.
Article26. Curtin BJ, Karlin DB. Axial length measurements and fundus changes of the myopic eye. Am J Ophthalmol. 1971; 1:42–53.
Article27. Grodum K, Heijl A, Bengtsson B. Refractive error and glaucoma. Acta Ophthalmol Scand. 2001; 79:560–6.28. Budenz DL, Anderson DR, Varma R, et al. Determinants of normal retinal nerve fiber layer thickness measured by Stratus OCT. Ophthalmology. 2007; 114:1046–52.
Article29. Ha DW, Sung K, Kim S, et al. Interocular comparison of nerve fiber layer thickness and its relation with optic disc size in normal subjects. Korean J Ophthalmol. 2002; 16:8–12.
Article30. Poinoosawmy D, Fontana L, Wu JX, et al. Variation of nerve fibre layer thickness measurements with age and ethnicity by scanning laser polarimetry. Br J Ophthalmol. 1997; 81:350–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reproducibility of Retinal Nerve Fiber Layer Thickness Evaluation by Nerve Fiber Analyzer
- Biometry of Retinal Nerve Fiber Layer Thickness by NFA
- Progression of Glaucoma in Highly Myopic Eyes with Paravascular Inner Retinal Defects
- Quantitative Analysis of Retinal Nerve Fiber Layer Thickness Profile in Myopic Eyes
- Influence of Diabetes Mellitus on the Retinal Ne rve Fiber Layer Thickness Measurement by Nerve Fiber Analyzer