Korean J Gastroenterol.
2013 May;61(5):243-251. 10.4166/kjg.2013.61.5.243.
The Role of Diet in Non-alcoholic Fatty Liver Disease
- Affiliations
-
- 1Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea. noshin@hanyang.ac.kr
- KMID: 1501645
- DOI: http://doi.org/10.4166/kjg.2013.61.5.243
Abstract
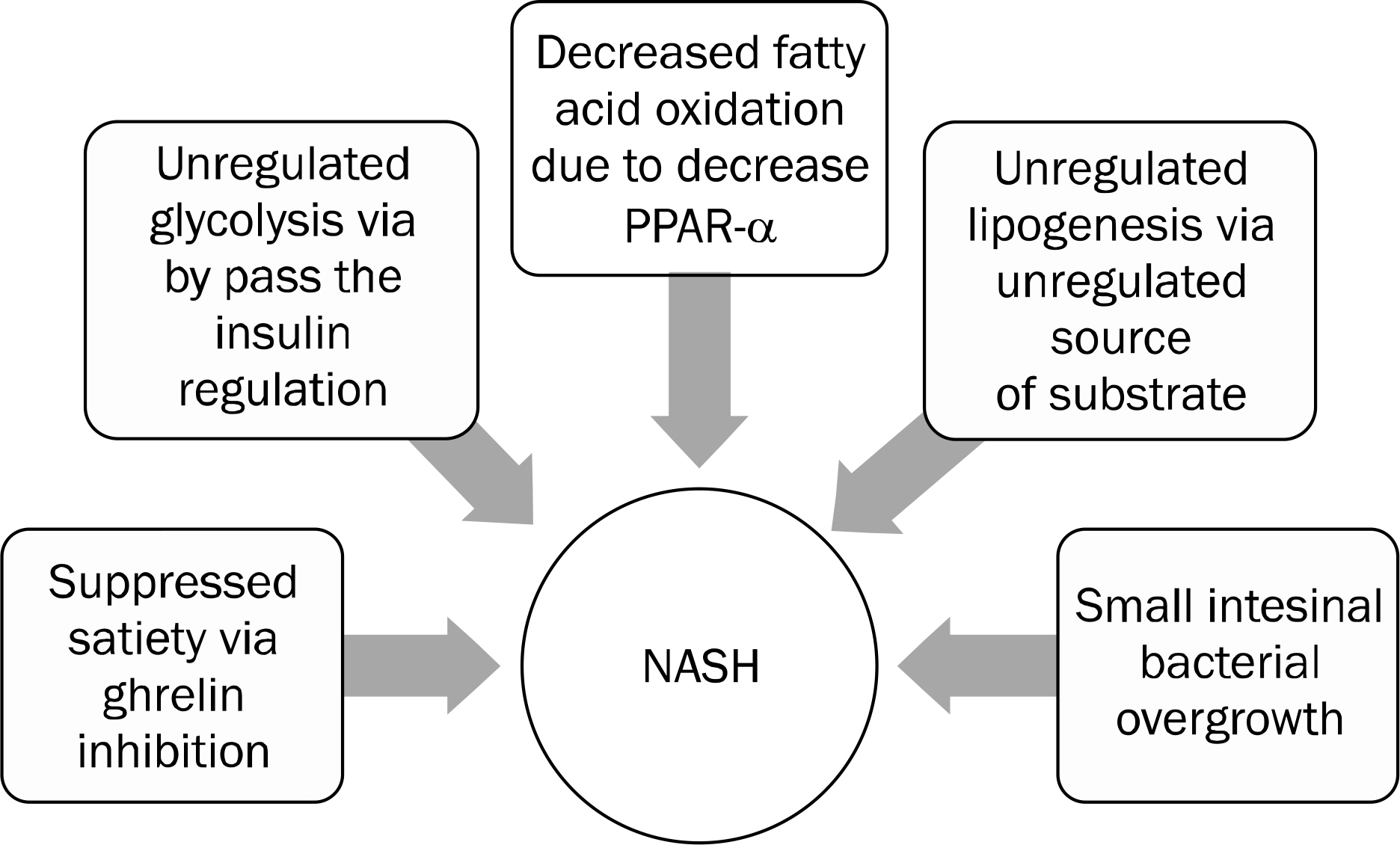
- Prevalence of non-alcoholic fatty liver disease (NAFLD) is about 20-25% in Korean adults population. Obesity is strongly associated with NAFLD and the prevention of obesity is a major public issue. Unfortunately, pharmacological treatment of obesity and NAFLD remains uncertain. Only weight loss by dietary changes been shown to lead to histological improvement in fatty liver. So the nutrition therapy is a cornerstone of treatment for NAFLD. Epidemiologic studies show that saturated fat, trans-fatty acid, carbohydrate, and simple sugar have strong correlation with intrahepatic fat accumulation. But, true associations with specific nutrients still remain unclear. Recently, fructose consumption has been rising in many countries and several epidemiologic studies show that fructose consumption has strong correlation with metabolic diseases. The consumption of excessively added sugar in the pathogenesis of steatohepatitis has received attention. Most clinicians agree with lifestyle modification are effective in histologic improvement. Total energy intake restriction is the most important action to reduce intrahepatic fat accumulation. Macronutrient composition may also have correlation with the development of NAFLD. To reduce the incidence of NAFLD, public statements on optimal dietary education program have been issused. Various specific dietary programs are suggested. Among them low fat diet and low carbohydrate diet are suggested in patients with NAFLD. However, there is no ideal diet to obtain the histological improvement in NAFLD. Further randomised controlled studies about specific diet are needed to determine the long-term benefit and histological improvement by ideal diet. Tailoring diet therapy to a patient's lifestyle is more important than universal specific dietary program.
MeSH Terms
Figure
Cited by 1 articles
-
A study on dietary habits, nutrient intakes and dietary quality in adults of a health screening and promotion center according to non-alcoholic fatty liver disease
Ji Ho Chang, Hye Seung Lee, Eun Hee Kang
J Nutr Health. 2014;47(5):330-341. doi: 10.4163/jnh.2014.47.5.330.
Reference
-
References
1. Ministry of Food and Drug Safety. Influence of dietary intake on non-alcoholic fatty liver disease in Korean. Cheongwon, Korea: Ministry of Food and Drug Safety;2012.2. Lee JY, Kim KM, Lee SG, et al. Prevalence and risk factors of non-alcoholic fatty liver disease in potential living liver donors in Korea: a review of 589 consecutive liver biopsies in a single center. J Hepatol. 2007; 47:239–244.
Article3. Speliotes EK, Massaro JM, Hoffmann U, et al. Fatty liver is associated with dyslipidemia and dysglycemia independent of visceral fat: the Framingham Heart Study. Hepatology. 2010; 51:1979–1987.
Article4. Rotman Y, Koh C, Zmuda JM, Kleiner DE, Liang TJ. NASH CRN. The association of genetic variability in patatin-like phospholi-pase domain-containing protein 3 (PNPLA3) with histological severity of nonalcoholic fatty liver disease. Hepatology. 2010; 52:894–903.
Article5. Speliotes EK, Yerges-Armstrong LM, Wu J, et al. GIANT Consortium; MAGIC Investigators; GOLD Consortium. Genome-wide association analysis identifies variants associated with non-alcoholic fatty liver disease that have distinct effects on metabolic traits. PLoS Genet. 2011; 7:e1001324.
Article6. Kechagias S, Ernersson A, Dahlqvist O, Lundberg P, Lindström T, Nystrom FH. Fast Food Study Group. Fast-food-based hyperalimentation can induce rapid and profound elevation of serum alanine aminotransferase in healthy subjects. Gut. 2008; 57:649–654.
Article7. Brøns C, Jensen CB, Storgaard H, et al. Impact of short-term high-fat feeding on glucose and insulin metabolism in young healthy men. J Physiol. 2009; 587:2387–2397.
Article8. Bortolotti M, Kreis R, Debard C, et al. High protein intake reduces intrahepatocellular lipid deposition in humans. Am J Clin Nutr. 2009; 90:1002–1010.
Article9. Westerbacka J, Lammi K, Häkkinen AM, et al. Dietary fat content modifies liver fat in overweight nondiabetic subjects. J Clin Endocrinol Metab. 2005; 90:2804–2809.
Article10. Musso G, Gambino R, De Michieli F, et al. Dietary habits and their relations to insulin resistance and postprandial lipemia in non-alcoholic steatohepatitis. Hepatology. 2003; 37:909–916.
Article11. Stamler J. Diet-heart: a problematic revisit. Am J Clin Nutr. 2010; 91:497–499.
Article12. Machado MV, Ravasco P, Jesus L, et al. Blood oxidative stress markers in non-alcoholic steatohepatitis and how it correlates with diet. Scand J Gastroenterol. 2008; 43:95–102.
Article13. Levy JR, Clore JN, Stevens W. Dietary n-3 polyunsaturated fatty acids decrease hepatic triglycerides in Fischer 344 rats. Hepatology. 2004; 39:608–616.
Article14. Cortez-Pinto H, Jesus L, Barros H, Lopes C, Moura MC, Camilo ME. How different is the dietary pattern in non-alcoholic steatohepatitis patients? Clin Nutr. 2006; 25:816–823.
Article15. Ahmed U, Redgrave TG, Oates PS. Effect of dietary fat to produce non-alcoholic fatty liver in the rat. J Gastroenterol Hepatol. 2009; 24:1463–1471.
Article16. Subramanian S, Goodspeed L, Wang S, et al. Dietary cholesterol exacerbates hepatic steatosis and inflammation in obese LDL receptor-deficient mice. J Lipid Res. 2011; 52:1626–1635.
Article17. Ibrahim A, Natrajan S, Ghafoorunissa R. Dietary trans-fatty acids alter adipocyte plasma membrane fatty acid composition and insulin sensitivity in rats. Metabolism. 2005; 54:240–246.
Article18. Tetri LH, Basaranoglu M, Brunt EM, Yerian LM, Neuschwan-der-Tetri BA. Severe NAFLD with hepatic necroinflammatory changes in mice fed trans fats and a high-fructose corn syrup equivalent. Am J Physiol Gastrointest Liver Physiol. 2008; 295:G987–G995.
Article19. Hession M, Rolland C, Kulkarni U, Wise A, Broom J. Systematic review of randomized controlled trials of low-carbohydrate vs. low-fat/low-calorie diets in the management of obesity and its comorbidities. Obes Rev. 2009; 10:36–50.
Article20. Hollingsworth KG, Abubacker MZ, Joubert I, Allison ME, Lomas DJ. Low-carbohydrate diet induced reduction of hepatic lipid content observed with a rapid non-invasive MRI technique. Br J Radiol. 2006; 79:712–715.
Article21. Muzio F, Mondazzi L, Harris WS, Sommariva D, Branchi A. Effects of moderate variations in the macronutrient content of the diet on cardiovascular disease risk factors in obese patients with the metabolic syndrome. Am J Clin Nutr. 2007; 86:946–951.
Article22. Nordmann AJ, Nordmann A, Briel M, et al. Effects of low-carbohy-drate vs low-fat diets on weight loss and cardiovascular risk factors: a metaanalysis of randomized controlled trials. Arch Intern Med. 2006; 166:285–293.23. Nseir W, Nassar F, Assy N. Soft drinks consumption and non-alcoholic fatty liver disease. World J Gastroenterol. 2010; 16:2579–2588.
Article24. Ouyang X, Cirillo P, Sautin Y, et al. Fructose consumption as a risk factor for non-alcoholic fatty liver disease. J Hepatol. 2008; 48:993–999.
Article25. Kang H, Greenson JK, Omo JT, et al. Metabolic syndrome is associated with greater histologic severity, higher carbohydrate, and lower fat diet in patients with NAFLD. Am J Gastroenterol. 2006; 101:2247–2253.
Article26. Solga S, Alkhuraishe AR, Clark JM, et al. Dietary composition and nonalcoholic fatty liver disease. Dig Dis Sci. 2004; 49:1578–1583.
Article27. Kwon OW, Jun DW, Lee SM, et al. Carbohydrate but not fat is associated with elevated aminotransferases. Aliment Pharmacol Ther. 2012. [Epub ahead of print].
Article28. Brinkworth GD, Noakes M, Keogh JB, Luscombe ND, Wittert GA, Clifton PM. Longterm effects of a high-protein, low-carbohy-drate diet on weight control and cardiovascular risk markers in obese hyperinsulinemic subjects. Int J Obes Relat Metab Disord. 2004; 28:661–670.
Article29. Cardillo S, Seshadri P, Iqbal N. The effects of a low-carbohydrate versus low-fat diet on adipocytokines in severely obese adults: three-year follow-up of a randomized trial. Eur Rev Med Pharmacol Sci. 2006; 10:99–106.30. Dansinger ML, Gleason JA, Griffith JL, Selker HP, Schaefer EJ. Comparison of the Atkins, Ornish, Weight Watchers, and Zone diets for weight loss and heart disease risk reduction: a randomized trial. JAMA. 2005; 293:43–53.
Article31. Foster GD, Wyatt HR, Hill JO, et al. A randomized trial of a low-car-bohydrate diet for obesity. N Engl J Med. 2003; 348:2082–2090.
Article32. Zelber-Sagi S, Nitzan-Kaluski D, Goldsmith R, et al. Long term nutritional intake and the risk for non-alcoholic fatty liver disease (NAFLD): a population based study. J Hepatol. 2007; 47:711–717.
Article33. Tovar AR, Torre-Villalvazo I, Ochoa M, et al. Soy protein reduces hepatic lipotoxicity in hyperinsulinemic obese Zucker fa/fa rats. J Lipid Res. 2005; 46:1823–1832.
Article34. Mikkelsen PB, Toubro S, Astrup A. Effect of fat-reduced diets on 24-h energy expenditure: comparisons between animal protein, vegetable protein, and carbohydrate. Am J Clin Nutr. 2000; 72:1135–1141.
Article35. Meyer TW, Anderson S, Brenner BM. Dietary protein intake and progressive glomerular sclerosis: the role of capillary hypertension and hyperperfusion in the progression of renal disease. Ann Intern Med. 1983; 98:832–838.
Article36. Lim JS, Mietus-Snyder M, Valente A, Schwarz JM, Lustig RH. The role of fructose in the pathogenesis of NAFLD and the metabolic syndrome. Nat Rev Gastroenterol Hepatol. 2010; 7:251–264.
Article37. Teff KL, Elliott SS, Tschöp M, et al. Dietary fructose reduces circulating insulin and leptin, attenuates postprandial suppression of ghrelin, and increases triglycerides in women. J Clin Endocrinol Metab. 2004; 89:2963–2972.
Article38. Nagai Y, Yonemitsu S, Erion DM, et al. The role of peroxisome pro-liferator-activated receptor gamma coactivator-1 beta in the pathogenesis of fructose-induced insulin resistance. Cell Metab. 2009; 9:252–264.39. Aigner E, Theurl I, Haufe H, et al. Copper availability contributes to iron perturbations in human nonalcoholic fatty liver disease. Gastroenterology. 2008; 135:680–688.
Article40. Bergheim I, Weber S, Vos M, et al. Antibiotics protect against fruc-tose-induced hepatic lipid accumulation in mice: role of endotoxin. J Hepatol. 2008; 48:983–992.
Article41. Sanyal AJ, Chalasani N, Kowdley KV, et al. Pioglitazone, vitamin E, or placebo for nonalcoholic steatohepatitis. N Engl J Med. 2010; 362:1675–1685.
Article42. Lavine JE, Schwimmer JB, Van Natta ML, et al. Effect of vitamin E or metformin for treatment of nonalcoholic fatty liver disease in children and adolescents: the TONIC randomized controlled trial. JAMA. 2011; 305:1659–1668.43. Gerss J, Köpcke W. The questionable association of vitamin E supplementation and mortality–inconsistent results of different meta-analytic approaches. Cell Mol Biol (Noisy-le-grand). 2009; 55(Suppl):OL1111–OL1120.44. Dietrich M, Jacques PF, Pencina MJ, et al. Vitamin E supplement use and the incidence of cardiovascular disease and all-cause mortality in the Framingham Heart Study: Does the underlying health status play a role? Atherosclerosis. 2009; 205:549–553.
Article45. Berry D, Wathen JK, Newell M. Bayesian model averaging in metaanalysis: vitamin E supplementation and mortality. Clin Trials. 2009; 6:28–41.
Article46. Zivkovic AM, German JB, Sanyal AJ. Comparative review of diets for the metabolic syndrome: implications for nonalcoholic fatty liver disease. Am J Clin Nutr. 2007; 86:285–300.
Article47. Benatti P, Peluso G, Nicolai R, Calvani M. Polyunsaturated fatty acids: biochemical, nutritional and epigenetic properties. J Am Coll Nutr. 2004; 23:281–302.
Article48. Parker HM, Johnson NA, Burdon CA, Cohn JS, O'Connor HT, George J. Omega-3 supplementation and non-alcoholic fatty liver disease: a systematic review and metaanalysis. J Hepatol. 2012; 56:944–951.
Article49. Panchal SK, Poudyal H, Waanders J, Brown L. Coffee extract attenuates changes in cardiovascular and hepatic structure and function without decreasing obesity in high-carbohydrate, high-fat diet-fed male rats. J Nutr. 2012; 142:690–697.
Article50. Vitaglione P, Morisco F, Mazzone G, et al. Coffee reduces liver damage in a rat model of steatohepatitis: the underlying mechanisms and the role of polyphenols and melanoidins. Hepatology. 2010; 52:1652–1661.
Article51. Birerdinc A, Stepanova M, Pawloski L, Younossi ZM. Caffeine is protective in patients with non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2012; 35:76–82.
Article52. Kim EK, Jun DW, Jang EC, Kim SH, Choi HS. Effect of coffee and green tea consumption on liver enzyme and metabolic syndrome in Korean. J Korea Acad Ind Coop Soc. 2012; 13:2570–2578.
Article53. Gressner OA, Lahme B, Rehbein K, Siluschek M, Weiskirchen R, Gressner AM. Pharmacological application of caffeine inhibits TGFbeta-stimulated connective tissue growth factor expression in hepatocytes via PPARgamma and SMAD2/3-dependent pathways. J Hepatol. 2008; 49:758–767.54. Ruhl CE, Everhart JE. Coffee and caffeine consumption reduce the risk of elevated serum alanine aminotransferase activity in the United States. Gastroenterology. 2005; 128:24–32.
Article55. Esposito K, Marfella R, Ciotola M, et al. Effect of a medi-terranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: a randomized trial. JAMA. 2004; 292:1440–1446.
Article56. Ryan MC, Itsiopoulos C, Thodis T, et al. The Mediterranean diet improves hepatic steatosis and insulin sensitivity in individuals with non-alcoholic fatty liver disease. J Hepatol. 2013. [Epub ahead of print].
Article57. Ventegodt S, Merrick E, Merrick J. Clinical holistic medicine: the Dean Ornish program ("opening the heart") in cardiovascular disease. ScientificWorldJournal. 2006; 6:1977–1984.
Article58. Haufe S, Engeli S, Kast P, et al. Randomized comparison of reduced fat and reduced carbohydrate hypocaloric diets on intrahepatic fat in overweight and obese human subjects. Hepatology. 2011; 53:1504–1514.
Article59. Korea Centers for Disease Control and Prevention. Korea Health Statistics 2010: Korea National Health and Nutrition Examination Survey. Cheongwon, Korea: KCDC;2010.60. Skilton MR, Laville M, Cust AE, Moulin P, Bonnet F. The association between dietary macronutrient intake and the prevalence of the metabolic syndrome. Br J Nutr. 2008; 100:400–407.
Article61. Cornier MA, Donahoo WT, Pereira R, et al. Insulin sensitivity determines the effectiveness of dietary macronutrient composition on weight loss in obese women. Obes Res. 2005; 13:703–709.
Article62. Ebbeling CB, Leidig MM, Feldman HA, Lovesky MM, Ludwig DS. Effects of a low-glycemic load vs low-fat diet in obese young adults: a randomized trial. JAMA. 2007; 297:2092–2102.63. Pittas AG, Das SK, Hajduk CL, et al. A low-glycemic load diet facilitates greater weight loss in overweight adults with high insulin secretion but not in overweight adults with low insulin secretion in the CALERIE Trial. Diabetes Care. 2005; 28:2939–2941.
Article64. Johnson NA, Sachinwalla T, Walton DW, et al. Aerobic exercise training reduces hepatic and visceral lipids in obese individuals without weight loss. Hepatology. 2009; 50:1105–1112.
Article65. Lazo M, Solga SF, Horska A, et al. Fatty Liver Subgroup of the Look AHEAD Research Group. Effect of a 12-month intensive lifestyle intervention on hepatic steatosis in adults with type 2 diabetes. Diabetes Care. 2010; 33:2156–2163.
Article66. Bonekamp S, Barone B, Clark JM, Stewarts KJ. The effect of an exercise training intervention on hepatic steatosis. Hepatology. 2008; 48(Suppl 1):806A.67. Harrison SA, Fincke C, Helinski D, Torgerson S, Hayashi P. A pilot study of orlistat treatment in obese, non-alcoholic steatohepatitis patients. Aliment Pharmacol Ther. 2004; 20:623–628.
Article68. Promrat K, Kleiner DE, Niemeier HM, et al. Randomized controlled trial testing the effects of weight loss on nonalcoholic steatohepatitis. Hepatology. 2010; 51:121–129.
Article69. Thoma C, Day CP, Trenell MI. Lifestyle interventions for the treatment of non-alcoholic fatty liver disease in adults: a systematic review. J Hepatol. 2012; 56:255–266.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Should you advocate for hepatocellular carcinomasurveillance in patients with alcohol-related liverdisease or non-alcoholic fatty liver disease?
- An Activation of Peroxisome Proliferator-Activated Receptor delta Attenuate Alcoholic Liver Disease and Nonalcoholic Fatty Liver Disease in Rats
- As sociation of Non-alcoholic Fatty Liver Disease with Metabolic Syndrome over 65 Years Elderly
- Association between a High-fat Low-carbohydrate Diet and Non-alcoholic Fatty Liver Disease: Truth or Myth?
- How to optimize the outcome of liver transplantation for non-alcoholic fatty liver disease