J Korean Endocr Soc.
2007 Jun;22(3):235-240. 10.3803/jkes.2007.22.3.235.
A Patient with Concurrent Medullary and Papillary Carcinoma of the Thyroid
- Affiliations
-
- 1Department of Internal Medicine, The Catholic University of Korea, College of Medicine, Korea.
- 2Department of Pathology, The Catholic University of Korea, College of Medicine, Korea.
- 3Department of Otolaryngology, The Catholic University of Korea, College of Medicine, Korea.
- KMID: 1512038
- DOI: http://doi.org/10.3803/jkes.2007.22.3.235
Abstract
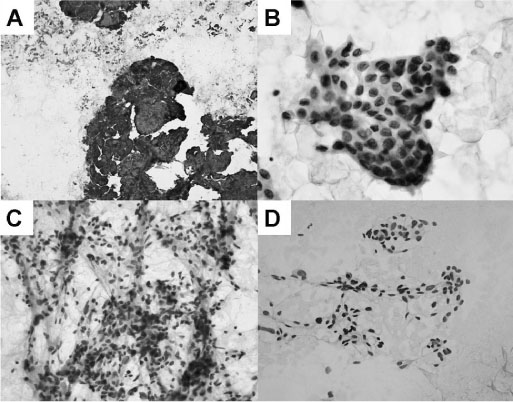
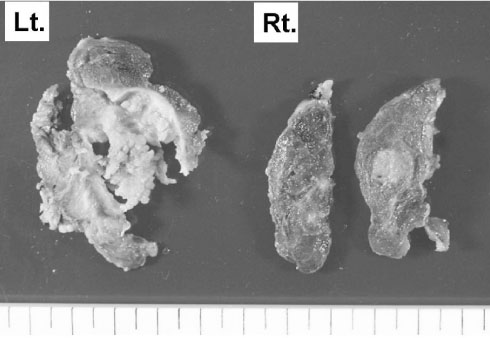
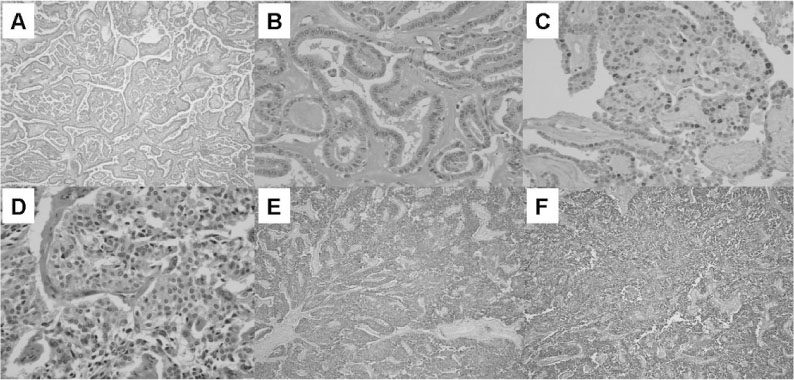
- The origin of medullary thyroid carcinoma and papillary thyroid carcinoma are embryogenically different, so these tumors have been thought to be independent of each other. We experienced a case of concurrent medullary and papillary thyroid carcinoma in one patient. The patient underwent total thyroidectomy and both two tumors were located at different lobes, respectively. Both tumors showed their own characteristic pathologic and immunohistochemical findings. The patient's elevated calcitonin level returned to the normal range after operation and there has been no evidence of recurrence. It is still controversial whether the concurrency is just coincidental or it arises from activation of a common tumorigenic pathway.
MeSH Terms
Figure
Cited by 1 articles
-
A Case of Concurrent Papillary and Medullary Thyroid Carcinomas Detected as Recurrent Medullary Carcinoma after Initial Surgery for Papillary Carcinoma
Ahn Dongbin, Ho Sohn Jin, Young Park Ji
J Korean Thyroid Assoc. 2013;6(1):80-84. doi: 10.11106/jkta.2013.6.1.80.
Reference
-
1. Nasir A, Chaudhry AZ, Gillespie J, Kaiser HE. Papillary microcarcinoma of the thyroid: a clinicopathologic and prognostic review. In Vivo. 2000. 14:367–376.2. Horn RC. Carcinoma of the thyroid. Description of a distinctive morphological variant and report 7 cases. Cancer. 1951. 4:697–707.3. Hazard JB, Hawak WA, Crile G Jr. Medullary (solid) carcinoma of the thyroid:, a clinicopathologic entity. J Clin Endocrinol Metab. 1959. 19:152–161.4. Hales M, Rosenau W, Okerlund MD, Galante M. Carcinoma of the thyroid with a mixed medullary and follicular pattern. Morphologic, immunohistochemical and clinical laboratory studies. Cancer. 1982. 50:1352–1359.5. Hedinger C, Williams ED, Sobin LH. The WHO histological classification of thyroid tumors: a commentary on the second edition. Cancer. 1989. 63:908–911.6. Ljungberg O, Ericsson UB, Bondeson L, Thorell J. A compound follicular-para follicular cell carcinoma of the thyroid: a new tumor entity. Cancer. 1983. 52:1053–1061.7. Galera-Davidson M, Fernandez A, Salguera M, Martin-Lacave I, Gonzalez-Campora R. Simultaneous hyperplasia of follicular and parafollicualr cells in experimental hypothyroidism. Lab Invest. 1988. 58:33A.8. Volante M, Papotti M, Roth J, Saremaslani P, Speel EJ, Lloyd RV, Carney JA, Heitz PU, Bussolati G, Komminoth P. Mixed medullary follicular thyroid carcinoma- Molecular evidence for dual origin of tumor components. Am J Pathol. 1999. 155:1499–1509.9. Nikiforov Y, Gnepp DR. Pediatric thyroid cancer after the Chernobyl disaster. Pathomorphologic study of 84 cases (1991-1992) from the Republic of Belarus. Cancer. 1994. 74:748–766.10. Albores-Saavedra J, Gorraez de la Mora T, de la Torre-Rendon F, Gouid E. Mixed medullary-papillary carcinoma of the thyroid: a previous unrecognized variant of thyroid carcinoma. Hum Pathol. 1990. 21:1151–1155.11. Shiroko T, Yokoo N, Okamoto K, Kitakado Y, Azuma H, Fukui T, Tanaka C. Mixed medullary-papillary carcinoma of the thyroid with lymph node metastasis: report of a case. Surg Today. 2001. 31:317–321.12. Lax SF, Beham A, Kronberger-Schonecker D, Langsteger W, Denk H. Coexistence of papillary and medullary carcinoma of the thyroid gland-mixed or collision tumor? Clinicopathological analysis or three cases. Virchows Arch. 1994. 424:441–447.13. Apel RL, Alpert LC, Rizzo A, LiVolsi VA, Asa SL. A metastasizing composite carcinoma or the thyroid with distinct medullary and papillary components. Arch Pathol Lab Med. 1994. 118:1143–1147.14. Tseleni-Balafouta S, Grigorakis SI, Alevizaki M, Karaiskos C, Davaris P, Koutras DA. Simultaneous occurrence of a medullary and papillary thyroid carcinoma in the same patient. Gen Diagn Pathol. 1997. 142:371–374.15. Merchant FH, Hirschowitz SL, Cohan P, Van Herle AJ, Natarajan S. Simultaneous occurrence of medullary and papillary carcinoma of the thyroid gland identified by fine needle aspiration: a case report. Acta Cytol. 2002. 46:762–766.16. Younes N, Shomaf M, Al Hassan L. Simultaneous medullary and papillary thyroid carcinoma with lymph node metastasis in the same patient: case report and review of the literature. Asian J Surg. 2005. 28:223–226.17. Shimizu M, Hirokawa M, LiVolsi VA, Mizukami Y, Harada T, Itoh T, Manabe T. Combined "mixed medullary-follicular" and "papillary" carcinoma of the thyroid with lymph node metastasis. Endocr Pathol. 2000. 11:353–358.18. Cuspisti K, Raffel A, Ramp U, Wolf A, Donner A, Krausch M, Eisenberger CF, Knoefel WT. Synchronous occurrence of a follicular, papillary and medullary thyroid carcinoma in a recurrent goiter. Endocr J. 2005. 52:281–285.19. Wu CJ, Chen HL, Song YM, Sheu WH, Chen SH. Mixed medullary-follicular carcinoma and papillary carcinoma of the same thyroid. Intern Med. 1998. 37:955–957.20. Hong SJ, Gong KY, Song YK, Ryu JS, Kim KS, Lee JH. Concurrent Medullary and papillary carcinoma of the thyroid. J Korean Soc Endocrinol. 1998. 13:634–639.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Concurrent Medullay and Papillary Carcinoma of the Thyroid
- Concurrent Papillary and Medullary Carcinoma of the Thyroid Gland
- A Case of Concurrent Papillary and Medullary Thyroid Carcinomas Detected as Recurrent Medullary Carcinoma after Initial Surgery for Papillary Carcinoma
- A Case of Concurrent Medullary and Papillary Carcinoma of the Thyroid Gland
- A Patient with Concurrent Medullary and Papillary Carcinoma of the Thyroid