Effects and Adequacy of High-Fidelity Simulation-Based Training for Obstetrical Nursing
- Affiliations
-
- 1Red Cross College of Nursing, Seoul, Korea.
- 2Department of Nursing, Namseoul University, Cheonan, Korea. aprilsea@hanmail.net
- KMID: 1018328
- DOI: http://doi.org/10.4040/jkan.2011.41.4.433
Abstract
- PURPOSE
Clinical training for nursing students is limited to rudimentary skills to avoid potential risks. Simulation-Based Training (SBT) can overcome the shortcomings of clinical training. We evaluated the educational effect of SBT for obstetrical nursing students using high-fidelity simulation courses.
METHODS
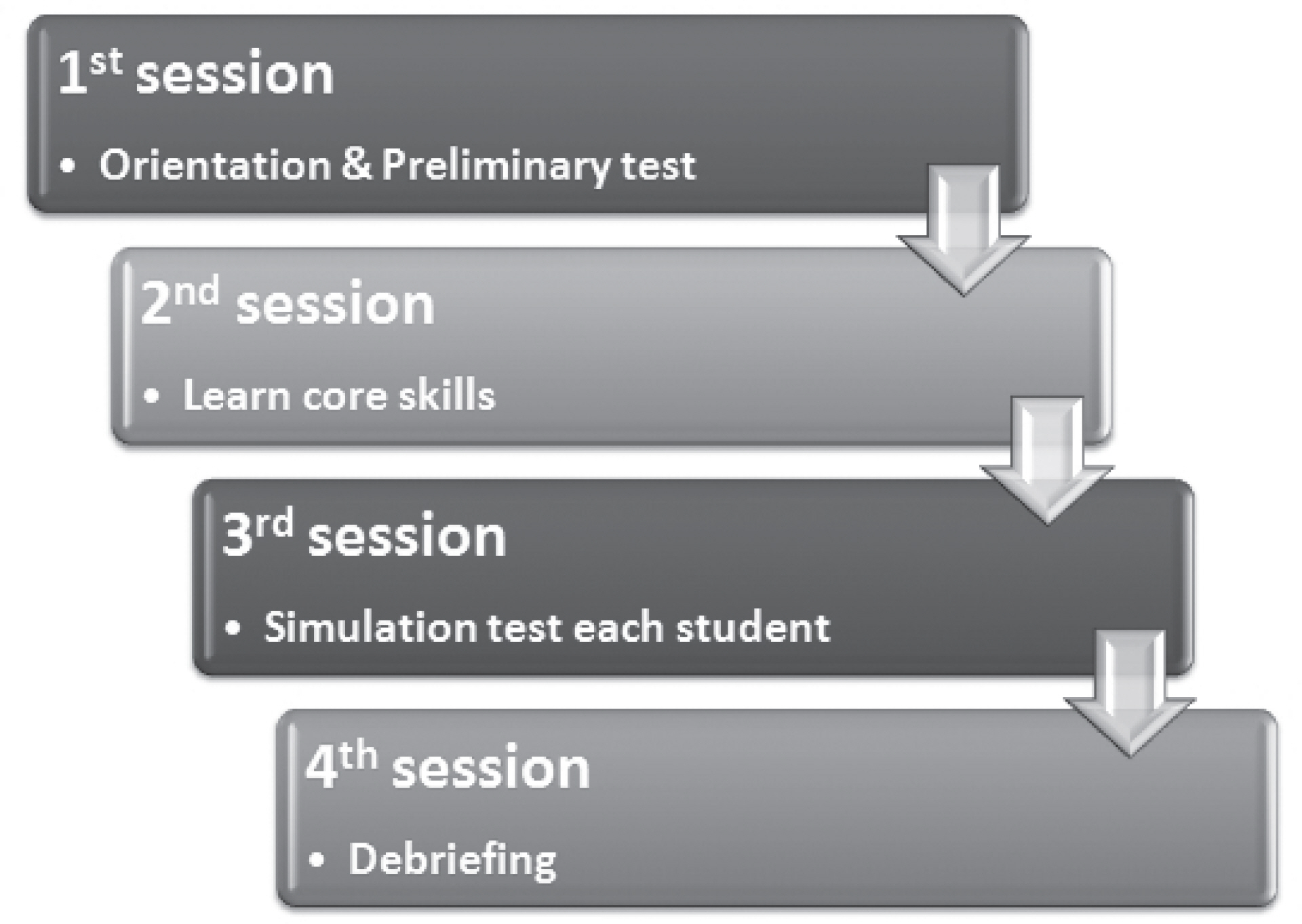
We developed a simulation program for obstetrical nursing students to practice nursing skills that are necessary to provide quality care. The program consisted of four sessions. 1st: An orientation and a preliminary test. 2nd: Learning core skills required in obstetrical nursing. 3rd: Testing each student with scenario. 4th: Providing a debriefing session. At the beginning of the program, students were surveyed about their self-confidence in obstetrical nursing care, and at the end of the program, they were surveyed about the adequacy of SBT as well as self-confidence.
RESULTS
Students' self-confidence showed a significant difference before and after simulation. Mean adequacy of SBT was 7.15+/-1.35 (out of 10). Most students became more interested in Women's Health Nursing after SBT.
CONCLUSION
The results from evaluating the effects of simulation-based obstetrical nursing training show that SBT provides invaluable clinical experience for obstetrical nursing students by overcoming the lack of actual clinical involvement in clinical training programs.
MeSH Terms
Figure
Cited by 10 articles
-
Effects of integrative simulation practice on nursing knowledge, critical thinking, problem-solving ability, and immersion in problem-based learning among nursing students
Young A Song
Korean J Women Health Nurs. 2020;26(1):61-71. doi: 10.4069/kjwhn.2020.03.15.1.Effects of Clinical Practice and Simulation-Based Practice for Obstetrical Nursing
Sun-Ae Kim, Sun-Kyung Lee, Hyun Ju Chae
Korean J Women Health Nurs. 2012;18(3):180-189. doi: 10.4069/kjwhn.2012.18.3.180.Effects of Simulation-based Education on Communication Skill and Clinical Competence in Maternity Nursing Practicum
Hye Young Kim, Eun Ko, Eun Sook Lee
Korean J Women Health Nurs. 2012;18(4):312-320. doi: 10.4069/kjwhn.2012.18.4.312.Current Status of Women's Health Nursing Practicum and Direction
Jeung-Im Kim, Heesun Kang, Somi Park, Sukhee Ahn
Korean J Women Health Nurs. 2014;20(2):173-183. doi: 10.4069/kjwhn.2014.20.2.173.Effect of Simulation-based Practice by applying Problem based Learning on Problem Solving Process, Self-confidence in Clinical Performance and Nursing Competence
Young A Song
Korean J Women Health Nurs. 2014;20(4):246-254. doi: 10.4069/kjwhn.2014.20.4.246.Development and Effects of Simulation Practice Program about Family centered Delivery Care
Seung Hee Yang, Sehoon Hong
Korean J Women Health Nurs. 2017;23(1):52-61. doi: 10.4069/kjwhn.2017.23.1.52.A Comparative Study on Learning Outcomes according to the Integration Sequences of S-PBL in Nursing Students: Randomized Crossover Design
So Young Yun, Ja Yun Choi
J Korean Acad Nurs. 2019;49(1):92-103. doi: 10.4040/jkan.2019.49.1.92.The effects of a maternal nursing competency reinforcement program on nursing students’ problem-solving ability, emotional intelligence, self-directed learning ability, and maternal nursing performance in Korea: a randomized controlled trial
Sun-Hee Kim, Bo Gyeong Lee
Korean J Women Health Nurs. 2021;27(3):230-242. doi: 10.4069/kjwhn.2021.09.13.Effect of Practical Delivery-nursing Simulation Education on Team-based Learning on the Nursing Knowledge, Self-efficacy, and Clinical Competence of Nursing Students
Sun Hee Lee
Korean J Women Health Nurs. 2018;24(2):150-162. doi: 10.4069/kjwhn.2018.24.2.150.
Reference
-
References
Alinier G., Hunt W &., Gordon R. 2004. Determining the value of simulation in nurse education: Study design and initial results. Nurse Education in Practice. 4:200–207. doi:10.1016/S1471(03)00066-0.
ArticleBaillie L &., Curzio J. 2009. Students’ and facilitators’ perceptions of simulation in practice learning. Nurse Education in Practice. 9:297–306. doi: 10.1016/j.nepr.2008.08.007.
ArticleBeaubien J M &., Baker D P. 2004. The use of simulation for training teamwork skills in health care: How low can you go? Quality & Safety in Health Care. 13:i51–i56.
ArticleChoi J Y., Jang K S., Choi S H &., Hong M S. 2008. Validity and reliability of a clinical performance examination using standardized patients. Journal of Korean Academy of Nursing. 38:83–91. doi:10.4040/jkan.2008.38.1.83.
ArticleCohen J. 1988. Statistical power analysis for the behavioral sciences. 2nd ed.Hillsdale, NJ: Erlbaum.
ArticleDeering S., Brown J., Hodor J &., Satin A J. 2006. Simulation training and resident performance of singleton vaginal breech delivery. Obstetrics & Gynecology. 107:86–89.
ArticleEllis D., Crafts J F., Hunt L P., Read M., Fox R &., James M. 2008. Hospital, simulation center, and teamwork training for eclampsia management: A randomized controlled trial. American Journal of Obstetrics and Gynecology. 111:723–731.Eom M R., Kim H S., Kim E K &., Seong K. 2010. Effects of teaching method using standardized patients on nursing competence in subcutaneous injection, self-directed learning readiness, and problem solving ability. Journal of Korean Academy of Nursing. 40:151–160. doi:10.4040/ jkan.2010.40.2.151.
ArticleFanning R M &., Gaba D M. 2007. The role of debriefing in simulation-based training. Society for Simulation in Healthcare. 2:115–125.Feltz D L. 1988. Self-confidence and sports performance. Exercise and Sport Sciences Reviews. 16:151–166. doi:10.1249/00003677-198800160-00016.
ArticleGardner R &., Raemer D B. 2008. Simulation in obstetrics and gynecology. Obstetrics and Gynecology Clinics of North America. 35:97–127. doi: 10.1016/j.ogc.2007.12.008.
ArticleGoffman D., Heo H., Chazotte C., Merkatz I &., Bernstein P S. 2008. Using simulation training to improve shoulder dystocia documentation. Obstetrics & Gynecology. 112:1284–1287.
ArticleHertel J P &., Millis B J. 2002. Using simulations to promote learning in higher education: An introduction. Sterling VA: Stylus.Jude D C., Gilbert C G &., Magrane D. 2006. Simulation training in the obstetrics and gynecology clerkship. American Journal of Obstetrics and Gynecology. 195:1489–1492. doi:10.1016/j.ajog.2006.05.003.
ArticleLasater K. 2007. High-fidelity simulation and the development of clinical judgement: Students’ experiences. Journal of Nursing Education. 46.Maslovitz S., Barkai G., Lessing J., Ziv A &., Many A. 2007. Recurrent obstetric management mistakes identified by simulation. Obstetrics & Gynecology. 109:1295–1300.
ArticleMcCaughey C S &., Traynor M K. 2010. The role of simulation in nurse education. Nurse Education Today. 30:827–832. doi:10.1016/j.nedt.2010.03.005.
ArticleMcIntosh J B., Alexander M., Veitch L &., May N. 1997. Evaluation of Nursing Times. 93:46–48.Mikkelsen J., Reime M H &., Harris A K. 2008. Nursing students’ learning of managing cross-infection scenario-based simulation training versus study groups. Nurse Education Today. 28:664–671. doi:10.1016/ j.nedt.2007.11.003.Mole L J &., McLafferty I H. 2004. Evaluating a simulated ward exercise for third year student nurses. Nurse Education in Practice. 4:91–99. doi: 10.1016/S1471(03)00031-3.
ArticleMoule P., Wilford A., Sales R &., Locker L. 2008. Student experiences and mentor views of the use of simulation for learning. Nurse Education Today. 28:790–797. doi:10.1016/j.nedt.2008.03.007.
ArticlePark H., Lee J., Hwang H., Lee J., Choi Y., Kim H. . 2003. The agreement of checklist recordings between faculties and standardized patients in an objective structured clinical examination (OSCE). Korean Journal of Medical Education. 15:141–150.
ArticlePark J H., Jung E., Ko J K &., Yoo H B. 2008. Delivery training for undergraduate medical students using birth simulator. Korean Journal of Obstetrics and Gynecology. 51:950–956.Park S I. 1998. Teory and practice of the teaching-learning method (II). Paju: Kyoyookbook.Pittini R., Oepkes D., Macrury K., Reznick R., Beyene J &., Windrim R. 2002. Teaching invasive perinatal procedures: Assessment of a high fidelity simulator-based curriculum. Ultrasound in Obstetrics and Gynecology. 19:478–483. doi:10.1046/j.1469-0705.2002.00701.x.
ArticleSiassakos D., Draycott T., Brien K., Kenyon C., Bartlett C &., Fox R. 2010. Exploratory randomized controlled trial of hybrid obstetric simulation training for undergraduate students. Te Journal of the Society for Simulation in Healthcare. 5:193–198. doi:10.1097/SIH.0b013e3181d3ee0b.
ArticleVu N V., Barrows H S., March M L., Verhulst S J., Colliver J A &., Travis T. 1992. Six years of comprehensive, clinical, performance-based assessment using standardized patients at the Southern Illinois University School of Medicine. Academic Medicine. 67:42–50. doi:10.1097/00001888-199201000-00009.
ArticleWilford A &., Doyle T J. 2006. Integrating simulation training into the nursing curriculum. British Journal of Nursing. 15:604–607.
ArticleYoo M S., Yoo L Y., Park Y O &., Son Y J. 2002. Comparison of students’ clinical competency in different instructional methods for fundamentals of nursing practicum. Journal of Korean Academy of Nursing. 32:327–335.
ArticleZiv A., Small S D &., Wolpe P R. 2000. Patient safety and simulation-based medical education. Medical Teacher. 22:489–495. doi:10.1080/01421590050110777.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects and Adequacy of High-Fidelity Simulation-Based Training for Obstetrical Nursing
- Effects of Web-based Simulation and High-fidelity Simulation of Acute Heart Disease Patient Care
- Development and effects of a labor nursing education program using a high-fidelity simulator for nursing students in Korea
- Comparison of Learning Effects using High-fidelity and Multi-mode Simulation: An Application of Emergency Care for a Patient with Cardiac Arrest
- Analysis of the virtual simulation practice and high fidelity simulation practice training experience of nursing students: A mixed-methods study