Tuberc Respir Dis.
2012 Jul;73(1):38-47. 10.4046/trd.2012.73.1.38.
Risk Factors Related with Mortality in Patient with Pulmonary Tuberculosis
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea. wonylee@yonsei.ac.kr
- KMID: 2050673
- DOI: http://doi.org/10.4046/trd.2012.73.1.38
Abstract
- BACKGROUND
The prevalence rate of pulmonary tuberculosis (PTB) is steadily decreasing in South Korea. However, PTB is a disease with relatively high mortality and morbidity rates throughout Korea. Although there are many studies and statistics about the risk factors of PTB mortality in many countries, there are only a limited number of domestic papers on this topic. The aim of this study is to determine predictive factors for mortality among in-hospital patients associated with PTB.
METHODS
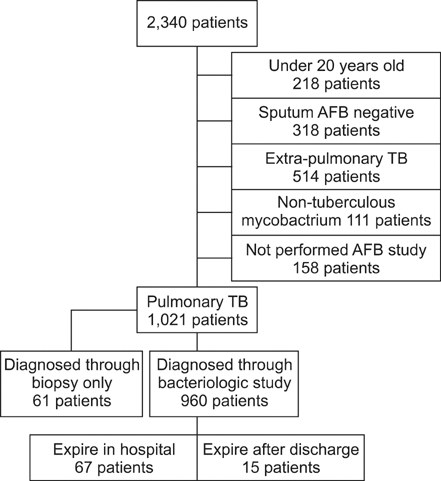
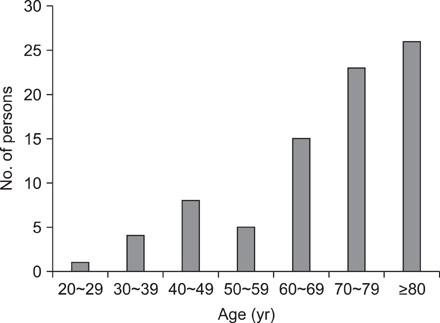
From December 2006 to January 2011, we reviewed medical records of 2,122 adult patients diagnosed with tuberculosis at a single tertiary hospital in a suburban area. In this study period, 960 patients were diagnosed with PTB by positive Acid fast bacilli smear and/or mycobacterial culture of the respiratory specimen. We compared the groups of patients deceased and patients discharged alive with PTB. The number of dead patients was 82 (47 males, 35 females).
RESULTS
Mortality was significantly associated with increased values of white blood cells (WBC), blood urine nitrogen (BUN), creatinine, C-reactive protein (CRP), numbers of involved lung field, and length of hospitalization. Also, it was associated with the decreased values of hemoglobin, lymphocyte, sodium, albumin, and cholesterol. Furthermore, admission through the emergency department, initial intensive care unit admission, and drug resistant PTB affected mortality in PTB patients. Independent predictors associated with PTB mortality are BUN, initial intensive care unit care, and admission during treatment of tuberculosis.
CONCLUSION
In our study, mortality of pulmonary tuberculosis was related with parameters associated with nutritional status, disease severity at the time of admission, and drug resistance.
Keyword
MeSH Terms
-
Adult
C-Reactive Protein
Cholesterol
Creatinine
Drug Resistance
Emergencies
Hemoglobins
Hospitalization
Humans
Intensive Care Units
Korea
Leukocytes
Lung
Lymphocytes
Male
Medical Records
Nitrogen
Nutritional Status
Prevalence
Republic of Korea
Risk Factors
Sodium
Tertiary Care Centers
Tuberculosis
Tuberculosis, Pulmonary
C-Reactive Protein
Cholesterol
Creatinine
Hemoglobins
Nitrogen
Sodium
Figure
Reference
-
1. World Health Organization. Report: global tuberculosis control. 2010. Geneva: World Health Organization.2. Statistics Korea [Internet]. c1996. cited 2011 Nov 17. Daejeon: Statistics Korea;Available from: http://kostat.go.kr/.3. Korean National Tuberculosis Association [Internet]. cited 2011 Nov 17. Seoul: Korean National Tuberculosis Association;Available from: http://www.knta.or.kr/.4. Harries AD, Hargreaves NJ, Gausi F, Kwanjana JH, Salaniponi FM. High early death rate in tuberculosis patients in Malawi. Int J Tuberc Lung Dis. 2001. 5:1000–1005.5. Davis CE Jr, Carpenter JL, McAllister CK, Matthews J, Bush BA, Ognibene AJ. Tuberculosis. Cause of death in antibiotic era. Chest. 1985. 88:726–729.6. Fine MJ, Auble TE, Yealy DM, Hanusa BH, Weissfeld LA, Singer DE, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997. 336:243–250.7. Lim WS, Macfarlane JT, Boswell TC, Harrison TG, Rose D, Leinonen M, et al. Study of community acquired pneumonia aetiology (SCAPA) in adults admitted to hospital: implications for management guidelines. Thorax. 2001. 56:296–301.8. Hong YP. Hong YP, Kim SJ, editors. Chapter 13. Clinical diagnostic classification. Tuberculosis. 1993. 4th ed. Seoul: The Korean Academy of Tuberculosis and Respiratory Diseases;142–143.9. Nguyen LT, Hamilton CD, Xia Q, Stout JE. Mortality before or during treatment among tuberculosis patients in North Carolina, 1993-2003. Int J Tuberc Lung Dis. 2011. 15:257–262.10. Nahid P, Jarlsberg LG, Rudoy I, de Jong BC, Unger A, Kawamura LM, et al. Factors associated with mortality in patients with drug-susceptible pulmonary tuberculosis. BMC Infect Dis. 2011. 11:1.11. Low S, Ang LW, Cutter J, James L, Chee CB, Wang YT, et al. Mortality among tuberculosis patients on treatment in Singapore. Int J Tuberc Lung Dis. 2009. 13:328–334.12. Lefebvre N, Falzon D. Risk factors for death among tuberculosis cases: analysis of European surveillance data. Eur Respir J. 2008. 31:1256–1260.13. Meintjes G, Schoeman H, Morroni C, Wilson D, Maartens G. Patient and provider delay in tuberculosis suspects from communities with a high HIV prevalence in South Africa: a cross-sectional study. BMC Infect Dis. 2008. 8:72.14. Mukadi YD, Maher D, Harries A. Tuberculosis case fatality rates in high HIV prevalence populations in sub-Saharan Africa. AIDS. 2001. 15:143–152.15. Shin SR, Kim CH, Kim SE, Park YB, Lee JY, Mo EK, et al. Predictors on in-hospital mortality following in-hospital diagnosis of tuberculosis. Tuberc Respir Dis. 2006. 61:233–238.16. Rao VK, Iademarco EP, Fraser VJ, Kollef MH. The impact of comorbidity on mortality following in-hospital diagnosis of tuberculosis. Chest. 1998. 114:1244–1252.17. Rasmussen TA, Søgaard OS, Camara C, Andersen PL, Wejse C. Serum procalcitonin in pulmonary tuberculosis. Int J Tuberc Lung Dis. 2011. 15:251–256.18. DeLegge MH, Drake LM. Nutritional assessment. Gastroenterol Clin North Am. 2007. 36:1–22.19. Goldwasser P, Feldman J. Association of serum albumin and mortality risk. J Clin Epidemiol. 1997. 50:693–703.20. Zahar JR, Azoulay E, Klement E, De Lassence A, Lucet JC, Regnier B, et al. Delayed treatment contributes to mortality in ICU patients with severe active pulmonary tuberculosis and acute respiratory failure. Intensive Care Med. 2001. 27:513–520.21. Kang JY, Kim MS, Kim JS, Kang HH, Kim SS, Kim YH, et al. Clinical characteristics and prognostic factors in patients with pulmonary tuberculosis admitted to intensive care units. Tuberc Respir Dis. 2010. 68:259–266.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Tuberculosis Verrucosa Cutis with Ulcer in a Patient with Pulmonary Tuberculosis
- Risk Factors Related with Mortality in Patient with Pulmonary Tuberculosis
- Tuberculosis Verrucosa Cutis in a Patient with Pulmonary Tuberculosis
- Hematological Study on Pulmonary Tuberculosis Patients
- Chronic Obstructive Pulmonary Disease: Respiratory Review of 2013