Tuberc Respir Dis.
2011 Aug;71(2):126-133. 10.4046/trd.2011.71.2.126.
Isolated Right Pulmonary Artery Hypoplasia with Retrograde Blood Flow in a 68-Year Old Man
- Affiliations
-
- 1Department of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. sdlee@amc.seoul.kr
- 2Department of Internal Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- 3Department of Radiology and Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 1846420
- DOI: http://doi.org/10.4046/trd.2011.71.2.126
Abstract
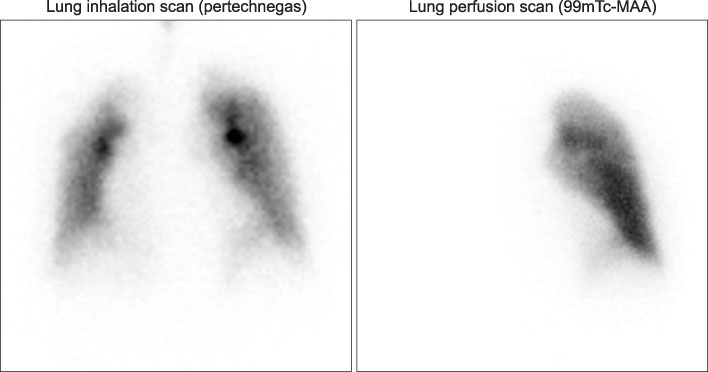
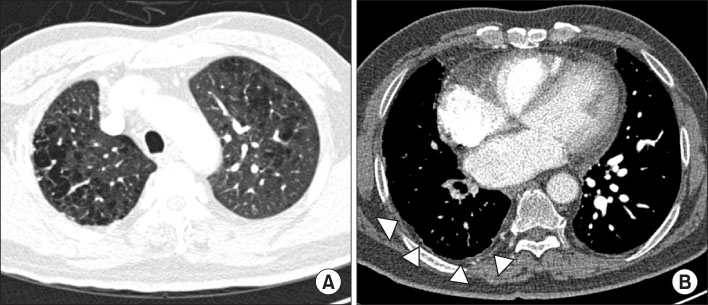
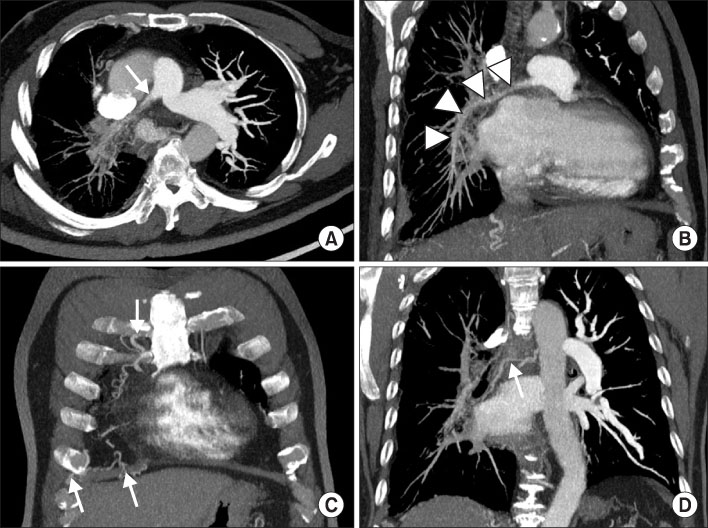
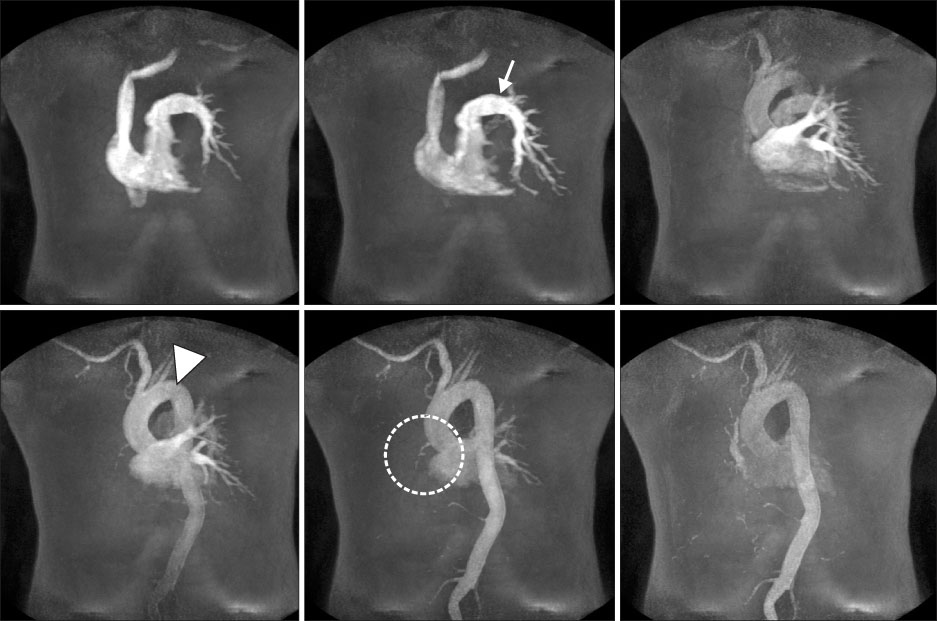
- Unilateral pulmonary artery hypoplasia (UPAH) is a rare disease in adults and is frequently accompanied by a congenital cardiac anomaly at a young age. The diagnosis is usually based on computed tomography (CT), angiography, and magnetic resonance imaging (MRI). However, no reports are available on retrograde flow in patients with UPAH. We describe a 68-year-old man with isolated UPAH and retrograde blood flow. He was admitted for dyspnea on exertion for the past 23 years. His diagnosis was delayed, as his symptoms and signs mimicked his underlying pulmonary diseases, such as emphysema and previous tuberculous pleurisy sequelae. A discrepancy was detected between the results of a ventilation-perfusion scan and the CT image. This was resolved by MRI, which showed retrograde blood flow from the right to the left pulmonary artery. Using MRI, we diagnosed this patient with isolated pulmonary artery hypoplasia and retrograde flow.
MeSH Terms
Figure
Reference
-
1. Ten Harkel AD, Blom NA, Ottenkamp J. Isolated unilateral absence of a pulmonary artery: a case report and review of the literature. Chest. 2002. 122:1471–1477.2. Bouros D, Pare P, Panagou P, Tsintiris K, Siafakas N. The varied manifestation of pulmonary artery agenesis in adulthood. Chest. 1995. 108:670–676.3. Rebergen SA, de Roos A. Congenital heart disease. Evaluation of anatomy and function by MRI. Herz. 2000. 25:365–383.4. Lynch DA, Higgins CB. MR imaging of unilateral pulmonary artery anomalies. J Comput Assist Tomogr. 1990. 14:187–191.5. Catala FJ, Martí-Bonmatí L, Morales-Marin P. Proximal absence of the right pulmonary artery in the adult: computed tomography and magnetic resonance findings. J Thorac Imaging. 1993. 8:244–247.6. Griffin N, Mansfield L, Redmond KC, Dusmet M, Goldstraw P, Mittal TK, et al. Imaging features of isolated unilateral pulmonary artery agenesis presenting in adulthood: a review of four cases. Clin Radiol. 2007. 62:238–244.7. Massumi RA, Donohoe RF. Congenital absence versus acquired attenuation of one pulmonary artery. Circulation. 1965. 31:436–447.8. Raymond BA, Forsee JH. Acquired unilateral pulmonary artery hypoplasia. Surgery. 1963. 53:579–586.9. Rees RS, Somerville J, Underwood SR, Wright J, Firmin DN, Klipstein RH, et al. Magnetic resonance imaging of the pulmonary arteries and their systemic connections in pulmonary atresia: comparison with angiographic and surgical findings. Br Heart J. 1987. 58:621–626.10. Isawa T, Taplin GV. Unilateral pulmonary artery agenesis, stenosis, and hypoplasia. Radiology. 1971. 99:605–612.11. Gluck MC, Moser KM. Pulmonary artery agenesis diagnosis with ventilation and perfusion scintiphotography. Circulation. 1970. 41:859–867.12. Steinberg I, Lyons HA. Ipsilateral hypoplasia of a pulmonary artery in advanced bronchiectasis. Am J Roentgenol Radium Ther Nucl Med. 1967. 101:939–946.13. Yacoub MH, Belcher JR, Attinson JN. Unilateral pulmonary artery hypoplasia associated with congenital cardiac anomalies. Br J Dis Chest. 1965. 59:102–112.14. Liebow AA, Hales MR, Lindskog GE. Enlargement of the bronchial arteries, and their anastomoses with the pulmonary arteries in bronchiectasis. Am J Pathol. 1949. 25:211–231.15. Lin YM, Liang KW, Ting CT. Unilateral pulmonary artery agenesis with presentation of hemoptysis: a case report. Zhonghua Yi Xue Za Zhi (Taipei). 1999. 62:644–647.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Isolated Right Pulmonary Artery Hypoplasia with Retrograde Blood Flow in a 68-Year Old Man
- Isolated Unilateral Pulmonary Artery Hypoplasia with Accompanying Pulmonary Parenchymal Findings on CT: A Case Report
- Blood flow velocity in the ascending aorta and main pulmonary artery of children by doppler echocardiography
- A Case of Left Pulmonary Artery Hypoplasia in Adult
- Persistent Truncus Arteriosus with Survival to the Age of 29 Years